Hormones of the adenohypophysis
- The gonadotropins, follicle-stimulating hormone and luteinizing hormone, exert their effects on the gonads (ovaries in the female and testes in the male). Taken together, the gonadotropins stimulate the gonads to:
- Produce gametes (ova and sperm)
- Secrete sex hormones (estrogen, progesterone, and testosterone)
- As the name suggests, follicle-stimulating hormone (FSH) stimulates the development in females of ovarian follicles.
- It is within the follicles that develop the ova, or eggs. This hormone also induces oestrogen secretion from the follicle.
- In males, FSH acts on the testicular Sertoli cells involved in the production of sperm. Luteinizing hormone (LH) is also referred to in the female for its effects that cause follicle rupture and ovum release and cause the ovarian follicle to be converted into a corpus luteum (Latin, yellow body).
- This hormone also induces the secretion of the corpus luteum of oestrogen and progesterone. LH acts on the Leydig cells of the testicles in males to stimulate testosterone secretion.
- The same cell type in the adenohypophysis produces FSH and LH: the gonadotrope. The release of FSH and LH is regulated by the GnRH (gonadotropin-releasing hormone) hypothalamic releasing hormone.
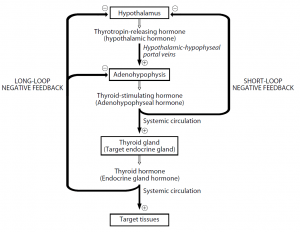
- The thyroid-stimulating hormone (TSH, thyrotropin) regulates the thyroid gland’s growth and metabolism. In addition, synthesis and release of the thyroid hormones, T3 and T4, are stimulated.
- Thyrotropin-releasinghormone (TRH) induces the release of TSH from the thyrotrope cells of the adenohypophysis. The adrenocorticotropic hormone (ACTH, adrenocorticotropin) stimulates the adrenal cortex to grow and produce steroids.
- Specifically, it stimulates cortisol secretion and other glucocorticoids involved in the metabolism of carbohydrates.
- More than one factor influences the release of ACTH from the adenohypophysis. The hypothalamus’s corticotropin-releasing hormone (CRH) stimulates the secretion of ACTH.
- In addition, with a peak in the early morning and a valley in the late afternoon, ACTH secretion follows a diurnal pattern.
- Prolactin (PRL), produced by adenohypophysis lactotrope cells, is involved in initiating and maintaining lactation in females.
- Its function in males is uncertain. Lactation involves three processes:
- Mammogenesis
- Lactogenesis
- Galactopoeisis
- Mammogenesis is the growth and growth of the milk-making mammary glands. In addition to PRL, this process requires the action of many hormones, including estrogens and progestins. The initiation of lactation is lactogenesis.
- Lactation is inhibited by high levels of estrogens and progestins during pregnancy. The levels of these two hormones fall at delivery, allowing lactation to be initiated by PRL.
- Galactopoeisis represents the maintenance of the production of milk. PRL and oxytocin require this process.
- The prolactin-inhibiting hormone (PIH, dopamine) from the hypothalamus normally inhibits the release of prolactin from the adenohypophysis.
- The secretion of prolactin is also regulated by the prolactin-releasing factor (PRF). Reflexes elicited by suckling and breast stimulation mediate the release of PRF from the hypothalamus.
- One of the few hormones that affects organs and tissues throughout the body is growth hormone (GH, somatotropin).
- This hormone is essential from birth until young adulthood for the normal growth and development of the skeleton as well as the visceral or soft tissues. Skeleton growth includes an increase in the thickness of bone and an increase in the length of bone.
- Stimulation of osteoblast (bone-forming cell) activity and proliferation of the epiphysal cartilage at the ends of the long bones are involved in the mechanism of this growth.
- Visceral tissue growth occurs through hyperplasia (increasing cell count) and hypertrophy (increasing cell size).
- By stimulating cell division and inhibiting apoptosis (programmed cell death) and cellular hypertrophy by promoting protein synthesis and inhibiting protein degradation, growth hormones cause hyperplasia.
- Somatomedins, which are peptides found in the blood, carry out the growth-promoting effects of GH. It identified and described two somatomedins.
- Structurally and functionally similar to insulin, these peptides are known as growth factors I and II (IGF-I and IGF-II) that are insulin-like.
- Growth hormone stimulates the liver to produce IGF-I, the predominant source of IGF-I found in the circulation. In many target tissues, local production of IGF-I also occurs.
- It is believed that IGF-I mediates GH’s growth-promoting effects throughout life. During puberty and other periods of growth in children, levels of GH and IGF-I rise in parallel.
- IGF-II production, by contrast, is not dependent on GH. Instead, during foetal growth and development, IGF-II is thought to be significant and is secreted in response to prolactin.
- The role of IGF-II in adults is ambiguous. In the body, growth hormone also has a lot of metabolic actions:
- Protein metabolism
- Increase in tissue amino acid uptake
- Stimulation of protein synthesis
- Lipid metabolism
- Increase in blood fatty acids
- Stimulation of lipolysis
- Inhibition of lipogenesis
- Carbohydrate metabolism
- Increase in blood glucose
- Decrease in glucose uptake by muscle
- Increase in the hepatic output of glucose (glycogenolysis)
- The net effects of these actions include improved growth due to protein synthesis; increased availability of fatty acids for skeletal muscle use as an energy source; and brain-sparing glucose, which can only be used as an energy source for this nutrient molecule.
- Two hypothalamic hormones govern the release of GH from adenohypophysis: growth hormone-releasing hormone (GHRH) and growth hormone-inhibiting hormone (GHIH, somatostatin).
- By stimulating or inhibiting the release of GHRH or by inhibiting GHIH release, any factor or condition that improves the secretion of GH could do so.
- GH secretion follows a daily rhythm with low and constant GH levels throughout the day and with a marked burst of GH secretion approximately one hour after sleep begins (deep or stage III and IV sleep).
- Exercise, stress, hypoglycemia, and increased serum amino acids, specifically arginine and leucine, are other factors that stimulate GH secretion.
- GH secretion inhibiting factors include hyperglycemia and ageing. In most people, after 30 years of age, GH production decreases.
- This decrease in the production of GH is probably a critical factor in the loss of 5 percent per decade of lean muscle mass and the gain of body fat at the same rate after 40 years of age.
REFERENCES:
RELATED TOPIC:
