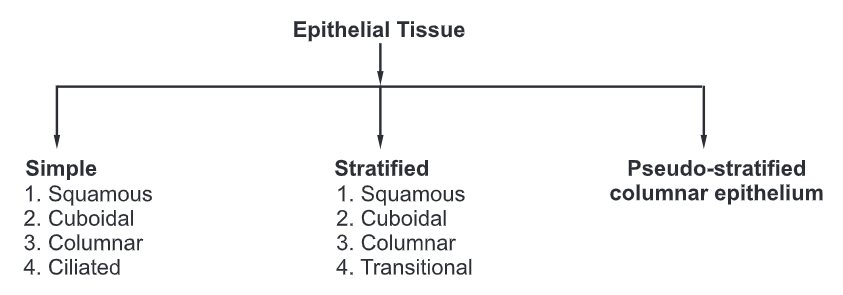
Epithelial Tissue
- An epithelial tissue or epithelium consists of cells arranged in continuous sheets, in either single or multiple layers.
- It covers body surfaces and lines hollow organs, body cavities, and ducts. It also forms glands.
Types of Epithelial Tissue
Functions of Epithelial Tissue:
- It protects the underlying tissue from friction and injury.
- It secret certain chemical substances that are utilized by the body.
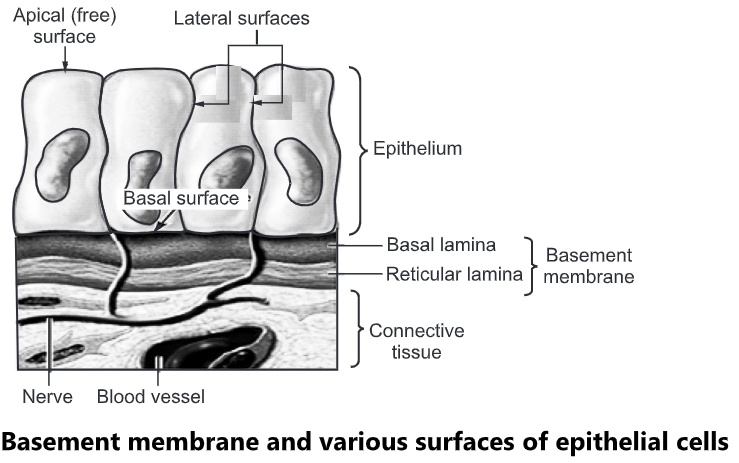
- On the basal side, the epithelial cells are supported by a basement membrane called as basal lamina.
- Below the basal lamina lies the capillary bed which provides the epithelium with the required nutrients and eliminates the waste products.
Surfaces of Epithelial Cells:
- Apical (free) surface: It faces the body surface. It may contain a body cavity, the lumen of an internal organ that receives cell secretions. It may contain cilia or microvilli.
- Lateral surface: It faces the adjacent cells on either side. It may contain tight junctions, adherens junctions, desmosomes, and/or gap junctions.
- Basal surface: It is present opposite to the apical surface. In multiple layers of epithelial cells, the apical layer is the most superficial layer of cells, and the basal layer is the deepest layer of cells.
Basement Membrane:
- It is a thin extracellular layer that consists of two layers, the basal lamina, and the reticular lamina.
- The basement membrane is a point of attachment and support for the overlying epithelial tissue.
- Basal lamina: It is closer to and secreted by the epithelial cells. It contains proteins such as laminin and collagen as well as glycoproteins and proteoglycans.
- Reticular lamina: It is closer to the underlying connective tissue and contains proteins such as collagen produced by connective tissue.
Simple Epithelium
It is made up of a single layer of cells and is divided into four types:
(a) Simple squamous epithelium
(b) Simple cuboidal epithelium
(c) Simple columnar epithelium
(d) Simple ciliated epithelium
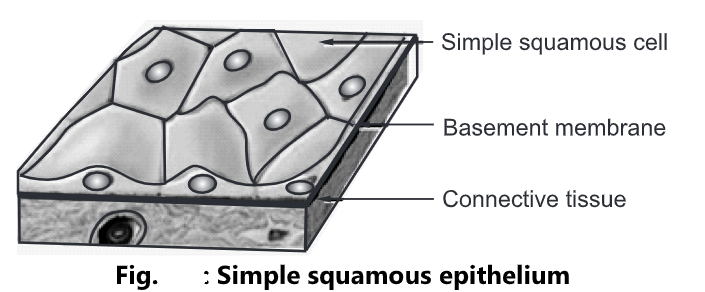
Simple Squamous Epithelium:
- It consists of a single layer of flat cells arranged on the basement membrane. The nucleus of each cell is oval or spherical and is centrally located.
- Location: It lines the heart, blood vessels, lymphatic vessels, air sacs of lungs and
the glomerular capsule of kidneys. - Functions: It performs the function of filtration (such as blood filtration in the kidneys), diffusion (such as diffusion of oxygen onto blood vessels of the lungs), and osmosis
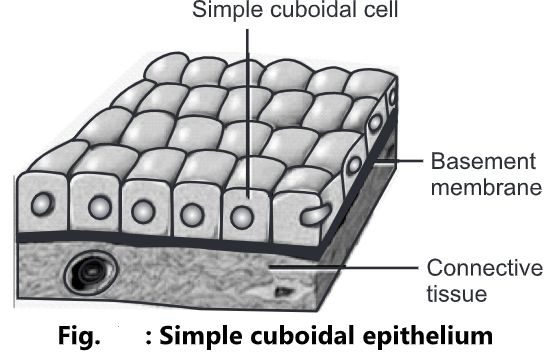
Simple Cuboidal Epithelium:
- It is made up of a single layer of cube-shaped cells arranged on the basement membrane.
- The nucleus of each cell is spherical in shape and is centrally located.
- Location: It lines the kidney tubules, pancreas and also forms the covering of ovaries.
- Functions: It performs the function of protection to the underlying tissues, secretion, and absorption of filtered substances.
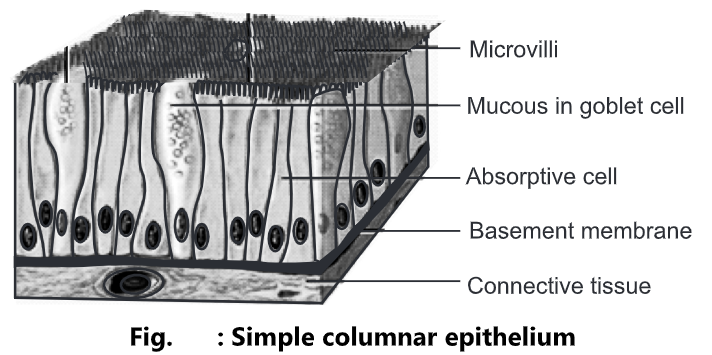
Simple Columnar Epithelium:
- It is made up of a single layer of rectangular cells arranged on the basement membrane.
- The nucleus of each cell is oval in shape and is located near the base of the cell. Mucous secreting columnar epithelium cells are called goblet cells.
- Location: It is the most abundant cell in the body. They are found in the nasal passage, eye, digestive system, reproductive system, ears, and buccal cavity.
- Functions: It performs the function of protection, secretion, providing sensory input, absorption, and transporting nutrients in the small intestine.
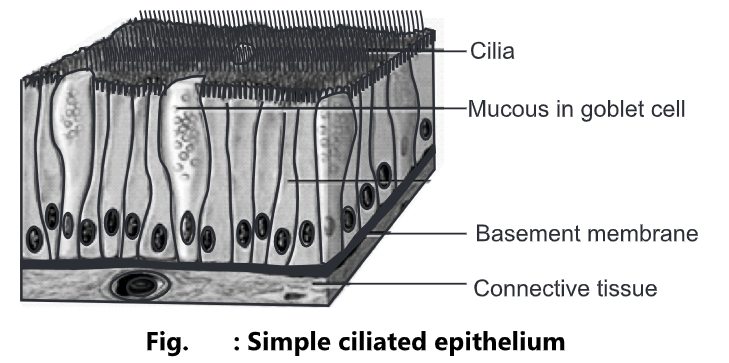
Simple Ciliated Epithelium:
- It is made up of columnar epithelial cells with many hair-like projections at the top called cilia. The nucleus of each cell is oval in shape and is located near the base of the cell. The cells are connected by tight junctions and desmosomes. The mucous secreting columnar epithelium cells are called as goblet cells.
- Location: It lines the upper respiratory tracts, uterine (fallopian) tubes, uterus, and central canal of the spinal cord.
- Functions: The cilia move the mucous and other substances by ciliary action. This prevents the adherence of any particulate matter such as bacteria, thus preventing infection. In the uterine tubes, the cilia propel the ova towards the uterus, and in the respiratory passages, they propel mucous towards the throat.
Stratified Epithelium
- It is made up of multiple layers of cells.
- It is further divided into four types.
- Stratified squamous epithelium
- Stratified cuboidal epithelium
- Stratified columnar epithelium
- Transitional epithelium
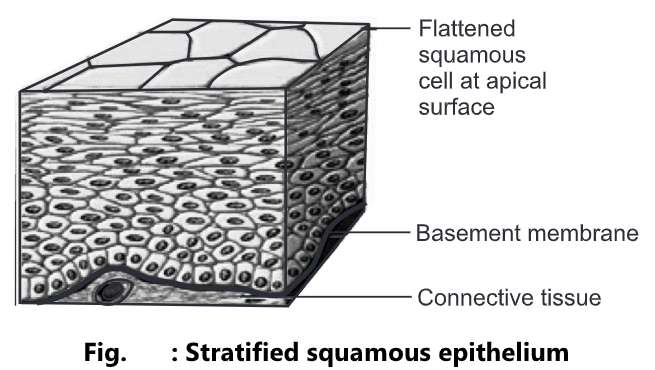
Stratified Squamous Epithelium:
- It is composed of more than one layer of cells having different shapes.
- The cells in the apical layer are flat and those present in deep layers vary in shape from cuboidal to columnar.
- As the cell grows their blood supply is restricted and they become dehydrated, shrunken, and harder.
- These issues exist in two forms keratinized and non-keratinized.
- In keratinized stratified squamous epithelium, the apical layer and several deep layers are dehydrated and contain a layer of keratin protein, a tough, fibrous protein that helps to protect the skin and underlying tissues from heat, microbes, and chemicals.
- In non-keratinized stratified squamous epithelium, keratin is absent from the apical layer and they remain moist.
- Location: Keratinized cells from the superficial layer of skin, Non-keratinized cells line the wet surfaces such as the lining of mouth, esophagus, part of epiglottis, vagina, and also covers the tongue.
- Functions: It gives protection against mechanical friction and chemical damage.
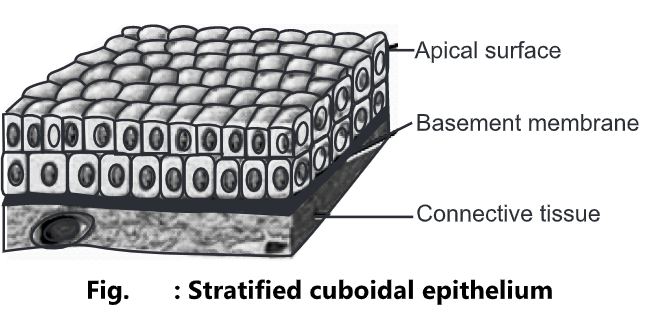
Stratified Cuboidal Epithelium:
- It is made up of two or more layers of cells. The cells in the apical layer are cuboidal in shape.
- Location: It lines the ducts of the sweat gland, male urethra, uterus, and anus.
- Functions: It plays an important role in protection, secretion, and absorption.
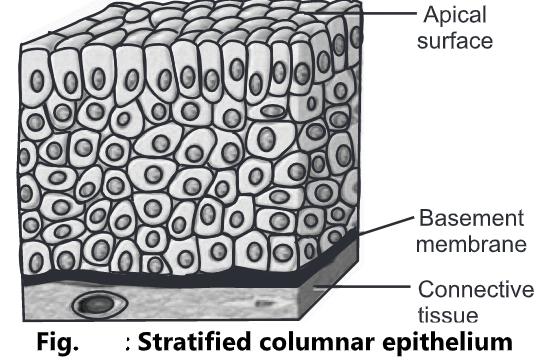
Stratified Columnar Epithelium:
- It is made up of several layers of irregularly shaped cells. In the apical layer, columnar cells are present.
- Location: It lines part of the urethra, large excretory ducts of glands, and conjunctiva of the eye.
- Functions: It performs the function of protection and secretion.
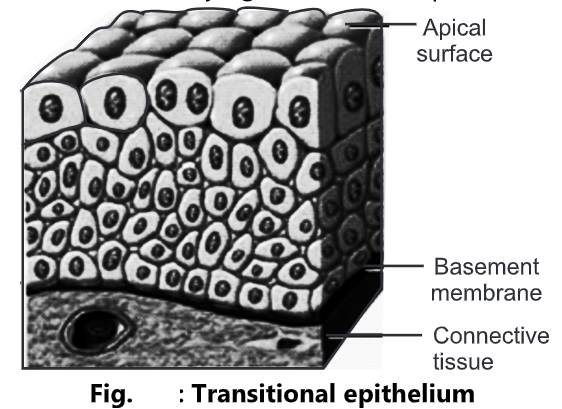
Transitional Epithelium:
- It consists of many layers of pear-shaped cells. The cells are variable in appearance.
- In a relaxed state, it looks like stratified cuboidal epithelium, and when stretched the cells become squamous shaped.
- Location: It lines the hollow organs such as the uterus and urinary bladder.
- Functions: It protects the underlying structure and permits the distension of organs.
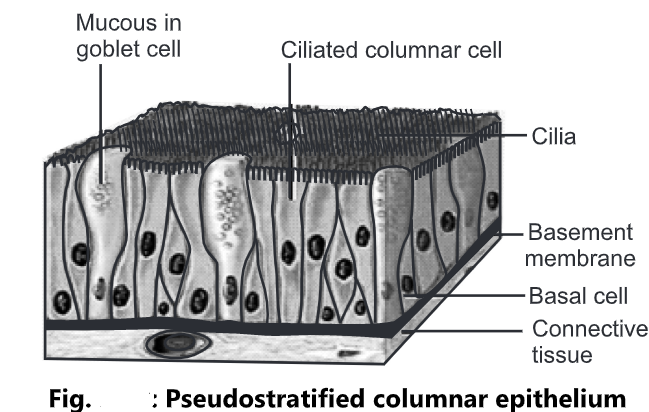
Pseudostratified Columnar Epithelium
- The cells are columnar in shape having a hair-like structure at the top called cilia.
- The nucleus is oval in shape and is present at different positions.
- All the cells are attached to the basement membrane, but not all reach the apical surface.
- Location: It lines the airways of the upper respiratory tract; pseudostratified non-ciliated columnar epithelium lines larger ducts of many glands, epididymis, and male urethra.
- Function: It functions in the secretion and movement of mucous by ciliary action.
Glandular Epithelium
- A gland may consist of a single cell or a group of cells.
- They are specialized cells that secrete substances into ducts.
- The glands are classified into endocrine or exocrine glands on the basis of their secretions.
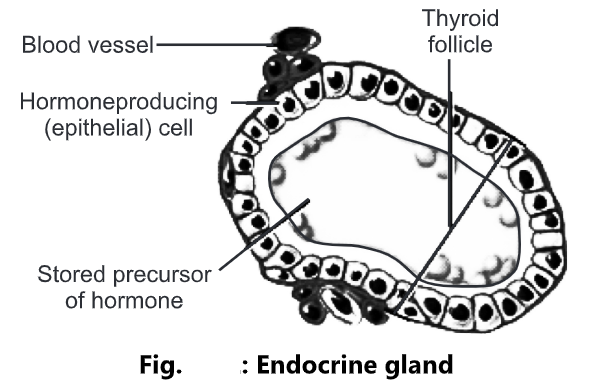
Endocrine gland:
- They are ductless glands.
- The secretions of endocrine glands enter the interstitial fluid and then diffuse directly into the bloodstream.
- These secretions are called hormones that regulate metabolic and physiological activities of the body in order to maintain homeostasis.
- Location: The pituitary gland, pineal gland, thyroid gland, parathyroid gland, adrenal glands, pancreas, ovaries, testes, and thymus are examples of endocrine glands.
- Function: The function of the endocrine gland is the production of hormones that regulate various metabolic and physiological activities.
- The pituitary gland secretes the human growth hormone responsible for the normal growth of individuals.
- The pineal gland secretes the melatonin hormone responsible for maintaining circadian rhythms and seasonal functions.
- The thyroid gland secretes T3 and T4 which are responsible for maintaining the normal functioning of the thyroid gland.
- The pancreas secretes the insulin hormone responsible for controlling the blood sugar level.
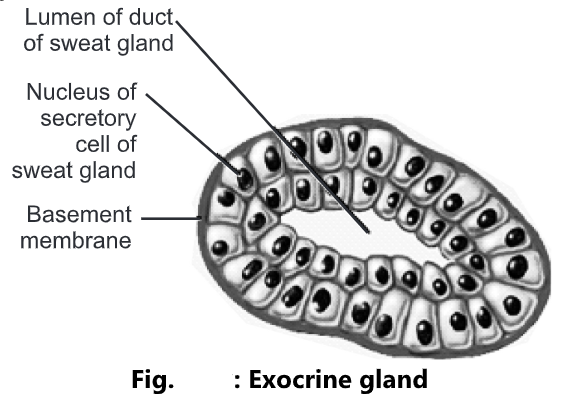
Exocrine Gland:
- These are the glands that possess ducts.
- The secretions of these glands are released into ducts that empty onto the skin surface or the lumen of a hollow organ.
- The secretions of exocrine glands include mucous, sweat, oil, earwax, saliva, and digestive enzymes.
- The secretory products of exocrine glands are released into the ducts.
- Examples of exocrine glands include sudoriferous (sweat) glands, which produce sweat that helps to reduce the body temperature, and salivary glands which secrete saliva.
- Location: They are present in the sweat gland, sebaceous gland, earwax glands, salivary glands, and pancreas
- Function: The function of exocrine glands in the production of sweat, oil, earwax, saliva, or digestive enzyme.
- Exocrine glands are classified as unicellular or multicellular on the basis of a number of cells.
Unicellular glands:
- These are composed of a single epithelial cell.
- They lack ducts.
- They secret their products directly on the surface of body cavities. For example, Goblet cells secrete mucous directly onto the apical surface of the intestinal tract.
Multicellular glands:
- These are composed of more than one cell.
- The epithelium grows down from the surface into the underlying tissues to form a simple or compound tube.
- It consists of an epithelium-derived duct and a secretory unit that is surrounded by connective tissue. E.g. Sudoriferous, sebaceous (oil), and salivary glands.
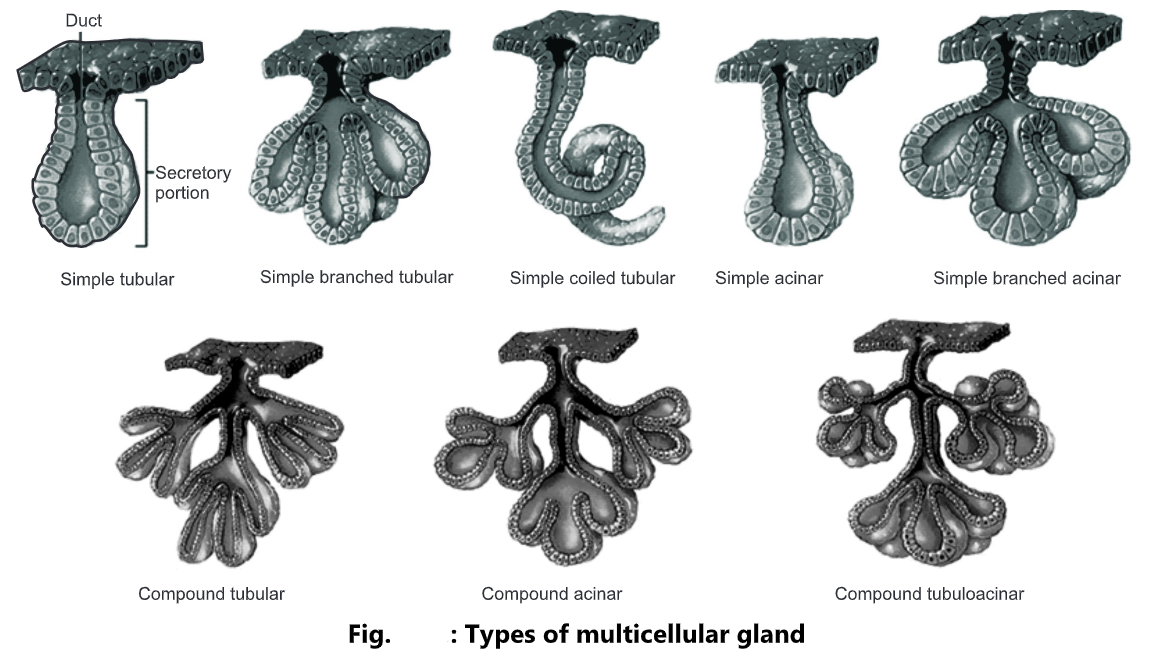
Types of Multicellular Gland:
On the basis of the structure of their ducts, multicellular exocrine glands are classified as:
Simple gland: If the duct of the gland does not branch it is called a simple gland.
Compound gland: If the duct of the gland is branched it is called a compound gland.
Tubular gland: If the duct of the gland is tubular in shape it is called a tubular gland.
Acinar gland: If the duct of the gland is rounded it is called as acinar gland.
Tubuloacinar gland: If the duct of the gland is both tubular and rounded it is called a tubuloacinar gland.
On the basis of their secretory unit, multicellular exocrine glands are classified as;
Simple glands:
- Simple tubular: Tubular secretory part is straight and attaches to a single unbranched duct. Example: Glands in the large intestine.
- Simple branched tubular: Tubular secretory part is branched and attaches to a single unbranched duct. Example: Gastric glands.
- Simple coiled tubular: Tubular secretory part is coiled and attaches to a single unbranched duct. Example: sweat glands.
- Simple acinar: Secretory portion is rounded and attaches to a single unbranched duct. Example: Glands of the urethra.
- Simple branched acinar: Rounded secretory part is branched and attaches to a single unbranched duct. Example: Sebaceous glands.
Compound Glands:
- Compound tubular: Secretory portion is tubular and attaches to a branched duct. Example: Bulbo-urethral glands.
- Compound acinar: Secretory portion is rounded and attaches to a branched duct. Example: Mammary glands.
- Compound tubuloacinar: Secretory portion is both tubular and rounded and attaches to a branched duct. Example: Acinar glands of the pancreas.