What is Cerebrospinal Fluid?
- Definition: Cerebrospinal fluid is a clear, colorless fluid found in the brain and spinal cord, acting as a cushion and medium for nutrient exchange within the CNS.
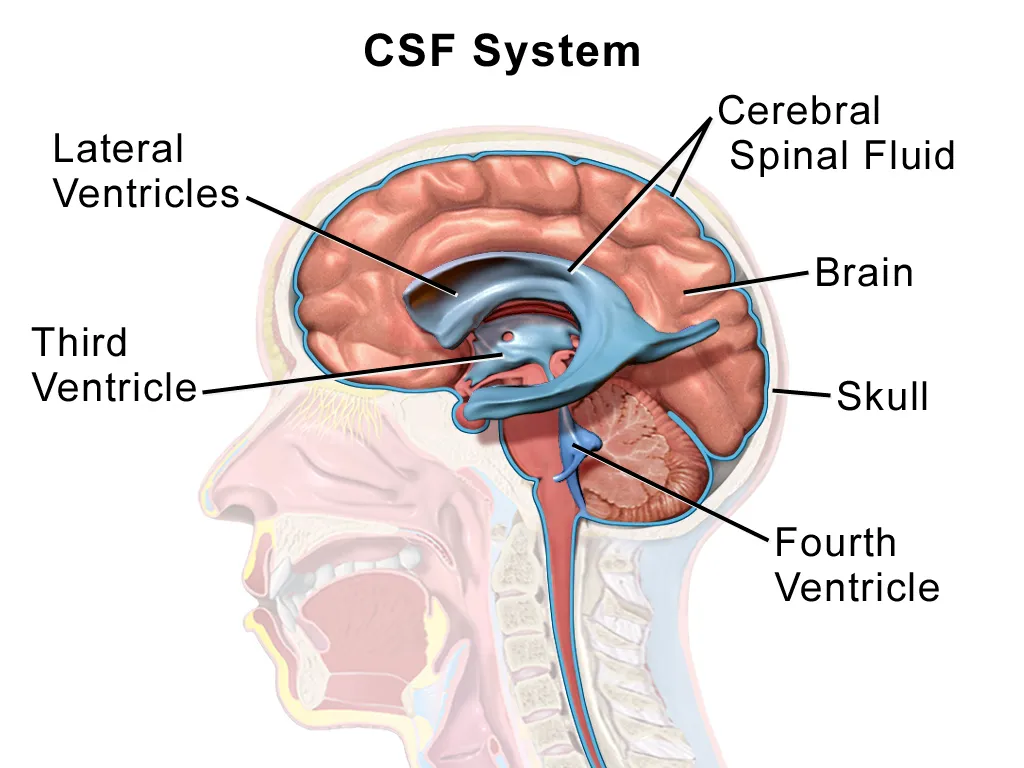
- Location: CSF is present in the ventricles of the brain, the subarachnoid space, and the central canal of the spinal cord.
- Volume: Approximately 125–150 mL of CSF is present in an adult human at any given time, with about 500 mL produced daily.
- Appearance: Transparent and watery, resembling plasma but with distinct compositional differences.
- Role in Diagnosis: CSF analysis is used to diagnose conditions like meningitis, multiple sclerosis, and brain tumors.
Composition of Cerebrospinal Fluid
The composition of CSF is tightly regulated to maintain the delicate environment of the CNS. Below is a detailed breakdown of its components, compared to blood plasma for clarity.
Key Components of CSF
- Water: Approximately 99% of CSF is water, providing its fluid nature.
- Electrolytes:
- Sodium (Na⁺): Maintains osmotic balance and neuronal excitability.
- Chloride (Cl⁻): Balances charge and pH.
- Potassium (K⁺): Supports neuronal function.
- Calcium (Ca²⁺) and Magnesium (Mg²⁺): Present in trace amounts, aiding synaptic activity.
- Proteins: Lower concentration than plasma (0.15–0.45 g/L vs. 60–80 g/L in plasma), including albumin, globulins, and transferrin.
- Glucose: Essential for brain metabolism, typically 50–80 mg/dL (about 60% of plasma glucose levels).
- Cells: Minimal presence, usually fewer than 5 white blood cells per microliter, with rare red blood cells.
- Other Substances: Lactic acid, urea, and trace amounts of neurotransmitters or metabolites.
Table 1: Comparison of CSF and Blood Plasma Composition
| Component | CSF | Blood Plasma |
|---|---|---|
| Water | ~99% | ~92% |
| Sodium (mEq/L) | 135–145 | 135–145 |
| Chloride (mEq/L) | 115–125 | 95–105 |
| Potassium (mEq/L) | 2.7–3.9 | 3.5–5.0 |
| Glucose (mg/dL) | 50–80 | 70–110 |
| Protein (g/L) | 0.15–0.45 | 60–80 |
| White Blood Cells | <5/µL | 4,000–11,000/µL |
| pH | 7.31–7.34 | 7.35–7.45 |
Factors Influencing Composition
- Production Site: Primarily produced by the choroid plexus, which filters plasma to create CSF.
- Blood-Brain Barrier: Regulates the passage of substances into CSF, ensuring low protein and cell content.
- Pathological Changes:
- Infections (e.g., meningitis): Increased proteins and white blood cells.
- Hemorrhage: Presence of red blood cells or xanthochromia (yellowish discoloration).
- Metabolic Disorders: Altered glucose levels, as seen in bacterial meningitis (low glucose).
Circulation of Cerebrospinal Fluid
CSF circulates through a well-defined pathway in the CNS, ensuring nutrient delivery and waste removal. The process involves production, flow, and absorption.
Production of CSF
- Primary Site: Choroid plexus, located in the lateral, third, and fourth ventricles.
- Mechanism:
- Filtration of plasma through fenestrated capillaries in the choroid plexus.
- Active transport of ions (Na⁺, Cl⁻) creates an osmotic gradient, drawing water into the ventricles.
- Rate: Approximately 20 mL/hour (500 mL/day), with constant turnover to maintain steady volume.
- Regulation: Controlled by the autonomic nervous system and hormones like atrial natriuretic peptide.
Pathway of CSF Circulation
- Ventricles:
- Lateral Ventricles: Two ventricles in the cerebral hemispheres produce most CSF.
- Third Ventricle: Receives CSF from lateral ventricles via the interventricular foramina (Monro).
- Fourth Ventricle: Connected to the third ventricle by the cerebral aqueduct (Sylvius).
- Subarachnoid Space:
- CSF flows from the fourth ventricle into the subarachnoid space via the foramina of Luschka and Magendie.
- Surrounds the brain and spinal cord, filling cisterns (e.g., cisterna magna).
- Central Canal: A small amount of CSF flows through the spinal cord’s central canal.
Absorption of CSF
- Primary Site: Arachnoid granulations (villi) in the superior sagittal sinus.
- Mechanism:
- CSF is absorbed into the venous blood through pressure-dependent diffusion.
- Lymphatic pathways in the nasal mucosa and spinal nerve roots also contribute.
- Rate of Absorption: Matches production to maintain stable intracranial pressure (ICP).
Table 2: CSF Circulation Pathway
| Stage | Location | Description |
|---|---|---|
| Production | Choroid Plexus | Filters plasma to produce CSF |
| Flow (Ventricles) | Lateral → Third → Fourth | Moves through ventricles via foramina |
| Subarachnoid Space | Brain and Spinal Cord | Bathes CNS, filling cisterns |
| Absorption | Arachnoid Granulations | Reabsorbed into venous blood |
Factors Affecting Circulation
- Obstructions: Tumors, cysts, or inflammation (e.g., meningitis) can block CSF flow, leading to hydrocephalus.
- Pressure Changes: Increased ICP (e.g., due to trauma) disrupts absorption, causing headaches or neurological symptoms.
- Aging: Reduced CSF production and absorption efficiency in older adults.
Functions of Cerebrospinal Fluid
CSF serves multiple critical functions, ensuring the brain and spinal cord operate optimally.
1. Mechanical Protection
- Cushioning Effect:
- Acts as a shock absorber, protecting the brain from impact against the skull.
- Reduces the effective weight of the brain (from ~1,400 g to ~50 g) via buoyancy.
- Stabilizing Structure: Maintains the brain’s position within the skull, preventing excessive movement.
2. Homeostasis and Nutrient Delivery
- Nutrient Supply:
- Delivers glucose and oxygen to neurons, supporting metabolic needs.
- Transports hormones and signaling molecules.
- pH Regulation: Buffers the CNS environment, maintaining a stable pH (7.31–7.34).
- Electrolyte Balance: Ensures optimal ion concentrations for neuronal signaling.
3. Waste Removal
- Clearance of Metabolites:
- Removes waste products like carbon dioxide, lactate, and excess neurotransmitters.
- Facilitates glymphatic system activity, clearing amyloid-beta (linked to Alzheimer’s disease).
- Detoxification: Prevents accumulation of harmful substances in the CNS.
4. Intracranial Pressure Regulation
- Pressure Maintenance:
- Balances CSF production and absorption to maintain normal ICP (5–15 mmHg in adults).
- Prevents brain compression or herniation.
- Pathological Implications: Abnormal CSF dynamics (e.g., hydrocephalus) can elevate ICP, causing neurological damage.
5. Immune Function
- Immune Surveillance:
- Contains low levels of immune cells (e.g., lymphocytes) to monitor for infections.
- Transports antibodies and immune mediators.
- Response to Infection: Changes in CSF composition (e.g., increased white blood cells) aid in diagnosing CNS infections.
Table 3: Functions of CSF
| Function | Description | Clinical Relevance |
|---|---|---|
| Mechanical Protection | Cushions brain, reduces weight via buoyancy | Prevents trauma-induced brain injury |
| Nutrient Delivery | Supplies glucose, oxygen, and ions | Supports neuronal metabolism |
| Waste Removal | Clears metabolites and toxins | Reduces risk of neurodegenerative diseases |
| ICP Regulation | Maintains stable intracranial pressure | Prevents hydrocephalus or herniation |
| Immune Function | Facilitates immune surveillance | Aids in diagnosing infections |
Clinical Significance of CSF
CSF analysis and dynamics are critical in diagnosing and managing neurological conditions.
CSF Analysis (Lumbar Puncture)
- Procedure:
- A needle is inserted into the subarachnoid space (L3-L4 or L4-L5) to collect CSF.
- Measures pressure, color, and composition.
- Indications:
- Infections (e.g., meningitis, encephalitis).
- Inflammatory diseases (e.g., multiple sclerosis).
- Subarachnoid hemorrhage or tumors.
- Findings:
- Bacterial Meningitis: Cloudy CSF, low glucose, high protein, high neutrophils.
- Viral Meningitis: Clear CSF, normal glucose, moderate protein, high lymphocytes.
- Subarachnoid Hemorrhage: Xanthochromia, red blood cells.
Disorders of CSF Dynamics
- Hydrocephalus:
- Obstructive: Blockage in ventricles (e.g., tumor) prevents CSF flow.
- Non-obstructive: Impaired absorption (e.g., post-hemorrhagic).
- Symptoms: Headache, nausea, cognitive impairment.
- Treatment: Ventriculoperitoneal shunt or endoscopic third ventriculostomy.
- Idiopathic Intracranial Hypertension:
- Elevated ICP without clear cause, often in young women.
- Symptoms: Headache, vision loss, papilledema.
- Treatment: Acetazolamide, weight loss, or shunting.
- CSF Leaks:
- Caused by trauma, surgery, or spontaneous defects.
- Symptoms: Positional headache, clear nasal discharge.
- Treatment: Bed rest, surgical repair.
FAQs About Cerebrospinal Fluid
- What is the main function of CSF?
- CSF protects the brain and spinal cord, delivers nutrients, removes waste, regulates intracranial pressure, and supports immune surveillance.
- How is CSF produced?
- CSF is primarily produced by the choroid plexus in the brain’s ventricles through filtration of blood plasma and active ion transport.
- What happens if CSF circulation is blocked?
- Blockage can lead to hydrocephalus, causing increased intracranial pressure, headaches, and potential brain damage.
- Why is CSF analysis important?
- It helps diagnose conditions like meningitis, multiple sclerosis, and hemorrhages by analyzing CSF composition and pressure.
- Can CSF leaks be dangerous?
- Yes, CSF leaks can lead to infections (e.g., meningitis) and low intracranial pressure, causing severe headaches.
- How does CSF differ from blood plasma?
- CSF has lower protein and cell content, slightly different electrolyte levels, and is tailored to the CNS environment.
