Bone And Connective Tissue In The Vertebrate Skeleton
Connective tissue
Connective tissue is abundant in the body: it is characterized by few cells, extensive intercellular mineral and/or protein, and a rich blood supply. It supports, protects and binds other cells together. Connective tissue comprises ‘connective tissue proper’, cartilage, bone and blood.
Connective tissue Proper
Connective tissue proper’ typically has elongated fibroblast cells and a more or less fluid intercellular material. There are five types:
(1) loose areolar tissue is found around organs, in mucous membranes and under the skin; hyaluronic acid is in the intercellular matrix with some fibers and cells;
(2) adipose tissue is areolar tissue with cells specialized for fat storage: it can grow throughout life;
(3) dense connective tissue has collagen fibers: it is found in tendons, ligaments, muscle fasciae, etc.;
(4) elastic connective tissue has branching elastic fibers: it is found in arterial walls, trachea, vocal cords, etc.;
(5) reticular connective tissue has a network of fibers: it forms the loose frame of the liver, spleen, lymph nodes, etc.
Cartilage Cartilage has a gel matrix containing chondrocytes and collagen and elastic fibers. It grows from within and without.
- Hyaline cartilage has a glassy consistency; it is found at the ends of bones, in the nose and the respiratory tract, and is supportive.
- Fibrocartilage is very strong. Strengthened with collagen, it connects bones (e.g. in the pelvis) and forms intervertebral disks (the relic of the notochord in most vertebrates).
- Elastic cartilage maintains the shapes of the external ear (pinna) and the larynx.
Bone
Bone is the main component of the skeletal system. Functions of bone (with cartilage) include:
- support (framework of body);
- protection (e.g. skull);
- leverage (limbs);
- mineral storage (especially calcium and phosphorus);
- storage of blood cell synthetic apparatus (red bone marrow: land vertebrates only);
- storage of energy (fat in yellow bone marrow: land vertebrates only).
Bone histology
Bone comprises many, widely separated cells surrounded by the intercellular matrix of bone tissue. Four principal bone cell types are found.
(1) Osteoprogenitor cells are stem cells which give rise to osteoblasts: they are found in the periosteum surrounding bones and in the endosteum membrane lining the inner bone cavity, also in canals in bone carrying blood vessels.
(2) Osteoblasts (on bone surfaces) secrete bone mineral and collagen.
(3) Osteocytes are osteoblasts within the bone matrix which they have built up around themselves; they maintain the functioning of bone.
(4) Osteoclasts (cells in the monocyte/macrophage series) resorb excess bone material. The bone matrix has collagen fibers and crystalline mineral (mainly hydroxyapatite, a hydrated calcium phosphate with some carbonate, fluoride, sulfate and magnesium salts). The protein collagen makes up about 33% of bone: the minerals crystallize around the protein framework. During aging, the proportion of protein in bone decreases, making it more brittle. Note that bone is a living tissue.
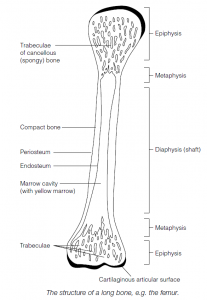
Bone morphology
A typical long bone (e.g. femur) comprises a shaft (diaphysis) and ends (epiphyses) connected by metaphyses. The cylindrical structure of a long bone concentrates most material around the periphery (as seen in cross-section), thus giving maximum resistance to bending moments. A thin layer of hyaline cartilage covers the epiphyses and reduces joint friction. The bone is covered by a periosteum: this has an outer fibrous layer (with nerves and blood vessels) and an inner osteogenic layer with bone-forming cells. In the middle (in higher, land vertebrates) is the marrow cavity, separated from the bone material by the endosteum.
Compact bone
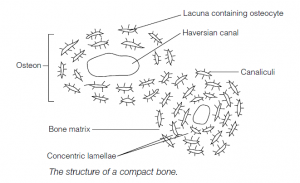
- Compact bone has few cavities within it; it covers spongy bone (see below) and is particularly thick in the shaft. It has a concentric ring structure .
- Vessels and nerves from the periosteum penetrate the bone via perforating canals and connect with nerves and vessels of the marrow cavity and the central Haversian canals which run longitudinally through the bone.
- Around the Haversian canals are concentric lamellae, rings of hard ‘bone’. Between the lamellae are small spaces, lacunae, containing osteocytes.
- Radiating from the lacunae are canaliculi which contain processes from the osteocytes and extracellular fluid; the canaliculi interconnect with each other and the Haversian canals.
- The Haversian canal plus the surrounding lamellae, lacunae, osteocytes and canaliculi form an osteon.
Spongy bone
Spongy (cancellous) bone lacks true osteons; it comprises an irregular lattice of thin plates (trabeculae). Within the trabeculae are lacunae with osteocytes. Spongy bone is rich in blood vessels and marrow lies within the network of trabeculae. The trabeculae are aligned parallel to the main forces of compression and tension in the bone.
Ossification
- Bone forms by osteogenesis (ossification), starting when mesenchymal cells in the embryo transform into osteoprogenitor cells which differentiate into osteoblasts and osteoclasts.
- Intramembranous ossification occurs within fibrous membranes of the embryo, fetus and child (e.g. skull bones). Clusters of osteoblasts accumulate on a fibrous matrix and deposit calcium salts.
- Endochondrial ossification occurs within a cartilage model, the primary ossification center being the shaft. Breakdown of cartilage results in cavitation: cavities merge to form a marrow cavity.
- Osteoblasts deposit mineral and protein, eventually replacing cartilage at the epiphyses where only the cartilaginous articular end-sheets remain together with the epiphyseal plates between the epiphyses and the shaft: the latter are the sites for bone growth.
Bone growth
- Bones elongate by appositional growth at the epiphyseal plates under hormonal control (e.g. growth hormone). New cartilage cells are generated on the epiphyseal side of the plate, and the older cartilage cells are destroyed and replaced by bone on the shaft side of the plate (thus the plate has a constant thickness but the length of the shaft increases).
- Growth in diameter occurs when osteoblasts from the periosteum add new bone to the outer surface of the bone while osteoclasts erode bone material inside the shaft and so enlarge the marrow cavity.
Modeling
- There is a homeostatic balance between formation and resorption of bone material, called remodeling. Calcium, phosphorus and vitamins C and D are essential.
- Overall bone growth is controlled by growth hormone from the anterior pituitary; calcitonin from the thyroid inhibits osteoclast activity; parathyroid hormone (parathormone, PTH) increases osteoclast activity; sex steroids promote a burst of bone growth during puberty followed by the destruction of the cartilage cells of the epiphyseal plates and epiphyseal fusion, with a cessation of bone growth in early adulthood.
- Bone mechanically stressed in exercise can increase its strength due to the generation of piezoelectric currents (from mineral crystals) which stimulate osteoblasts. In aging, calcium is withdrawn from bones with a tendency towards osteoporosis; less collagen makes aged bones more brittle.
Joints
Joints are points of contact between bones (or cartilage and bone) allowing for varying degrees of movement, from none to freely movable.
- Fibrous joints: bones are held together with fibrous connective tissue. A fibrous joint permits minimal movement, for example sutures between skull bones, articulation of teeth in jaws.
- Cartilaginous joints: bones are held tightly together by cartilage and permit minimal movement. Examples are epiphyseal plates within bones and the pubic symphysis between the two halves of the pelvis.
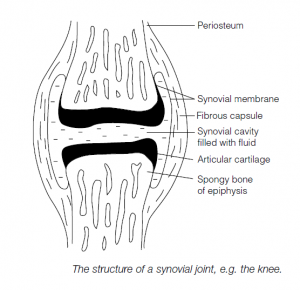
- Synovial joints: these allow movement. There is a synovial cavity between bones; hyaline cartilage covers the ends of the articulating bones. Joints are surrounded by a sleeve capsule with an outer, fibrous dense connective tissue layer attached to the periosteum. If the fibers are arranged in parallel bundles they are called ligaments. The inner capsule layer is the synovial membrane of looser connective tissue: this secretes a lubricating synovial fluid. Pads of fibrocartilage (articular disks on the articular surfaces of the bones) may be present within the synovial capsule. (Similar capsules, bursae, may be found in the body at sites of friction, e.g. where skin rubs over bone.)
Movements of Joints
Joints may be further categorized into:
- gliding joints (usually flat, e.g. ribs over vertebrae);
- hinge joints (angular movement, e.g. elbow);
- pivot joints (rotation, e.g. atlas vertebra allowing head-shaking);
- ellipsoidal joints (side-to-side or back-and-forth, e.g. wrist);
- saddle joints (freer version of ellipsoidal joint, e.g. base of thumb);
- universal joints (ball-and-socket, e.g. hip).
