Diuretics are the agents which increase the rate and volume of urine formation. These agents mainly act on nephrons and promotes the excretion of excess fluid.
These are indicated in the treatment of (a) edema due to a variety of reasons, (b) hypertension and (c) drug poisoning to promote its excretion.
Classification of Diuretics :
Diuretics can be classified into the following four categories :
(I) Weak Diuretics: It is divided further divided into four categories:
(a) Osmotic diuretics : (i) Electrolytes. e.g. Sodium and Potassium salts, (ii) Non-electrolytes. e.g. Mannitol.
(b) Acidifying salts. e.g. Ammonium chloride.
(c) Xanthine derivatives. e.g. Aminophylline.
(d) Carbonic anhydrase inhibitors. e.g. Acetazolamide.
(II) Moderately Potent Diuretics : e.g. Benzothiadiazine.
(III) Very Potent Diuretics : e.g. Parenteral organic mercurials e.g. Frusemide ethacrynic acid.
(IV) Potassium Sparing Diuretics : e.g. Triameterene. Aldosterone antagonist, Spironolactone.
Water as a Diuretic :
Water given in excess can act as diuretic. In this case, the antidiuretic hormone (ADH) remains inhibited and nephron becomes permeable to water. In water diuresis, water is removed from body greatly in excess of solute. In oedema, major problem is sodium retention, the water retention being secondary in such case. Water does not act as a good diuretic. Water diuresis is recommended to wash out certain drugs which irritate the urinary tract or are of limited solubility in urine such as salicylates, sulphonamide. It is also useful in urinary tract infections.
(1) Weak diuretics
(a) Osmotic Diuretics :
(i) Electrolytes: The capacity of tubules to reabsorb osmotically active substances is limited. If in plasma one of such solute is increased then its concentration in glomerular filtrate also increases. This increase in the concentration of solute in the tubular fluid opposes the reabsorbtion of water by osmotic activity and act as a osmotic diuretic. This increase in excretion of such solute increases excretion of water. Thus, osmotic diuretic should not get metabolised in the body and should not get reabsorbed by renal tubules.
(1) Sodium Chloride (NaCl): Excess of NaCl causes osmotic diuresis. Intravenous administration of hypertonic NaCl solution raises solute concentration of extra-cellular fluid and of glomerular filtrate leading to diuresis. Sodium salts are however weak in action as Na+ is reabsorbed. In case of oedema where diuretics are indicated there is already excess of Na+ in body and sodium salts aggravate the condition. NaHCO3 is sometimes used to produce alkaline urine. e.g. In urinary tract infections and in sulphonamide administration.
(2) Potassium Salts: These are more effective than sodium salts. Potassium citrate is commonly used to produce alkaline urine. Administration of potassium salts in presence of renal insufficiency causes hyperkalemia.
(ii) Non-electrolytes :
Mannitol : Mannitol is a sugar. When hypertonic solution of mannitol is injected; draws water from the cells and extracellular spaces into the vessels. Plasma volume is increased enhancing renal blood flow and diuresis occurs by increase in osmotic pressure of the glomerular filtrate so that tubular reabsorption of water is diminished. It is used as diuretic to treat oliguric condition of acute renal failure. It is also used to reduce intraocular pressure.
(b) Acidifying Salts :
Ammonium Chloride (NH4 Cl): It is given orally. After absorption it is converted by liver into urea and H+ ion is formed.
NH4CI → NH3+ H+ + Cl–
The H+ ion reacts with bicarbonate and other buffers in extracellular fluid. Reduction in bicarbonate causes acidosis and fall in extracellular pH of tubular cells. This is believed to cause diuresis and urine becomes acidic. The excess Cl ions from ECF are filtered by glomerulus and promotes osmotic diuresis. The diuretic action of ammonium chloride is self-limiting as kidney compensates for acidosis by producing ammonia gas by secreting more H+ for exchanging with Na+ in the tubular fluid. The excess of Cl– filtered is excreted in combination as NH4Cl.
Adverse Reactions :
Nauseous taste, gastric irritation causes nausea and vomiting. In presence of renal damage it causes acidosis.
Therapeutic Uses :
Drug is not used as diuretic but is used as urinary acidifying agent. Dose 8-12 gm daily in divided doses.
(c) Xanthine Derivatives :
Theophylline: It is best diuretic and is generally used as Aminophylline. Xanthines probably act by increasing the renal blood by both cardiac and vascular actions, as well as by inhibiting tubular reabsorbtion of sodium. It is weak diuretic but in order to increase its effectivity it should be given by intravenous route, slowly in the dose of 0.25 to 0.5 diluted in 10 to 20 ml of 5% glucose solution.
(d) Carbonic Anhydrase Inhibitors :
Acetazolamide: It acts by inhibiting the enzyme carbonic anhydrase.
Pharmacological Actions :
(1) Kidney and Electrolytes: Carbonic anhydrase is present in renal cortex. It catalyses the reaction.
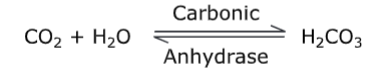
This H2CO3 formed dissociates to give H+and HCO3– . This H+is made available for exchange with Na+. Thus, the enzyme plays an important role in tubular reabsorption of sodium.
Acetazolamide inhibits this enzyme by non-competitive mechanism so that H+ is not made available for exchange with Na+. Hence, Na+ along with water is excreted. H+ ion combines with HCO3 provided by glomerular filtrate to form H2CO3– which is converted to water and carbon dioxide. The carbon dioxide formed is absorbed. Thus, in acetazolamide therapy due to lack of H++ the H2CO3– is excreted in large amount, the urine becomes alkaline. Since, there is lack of H+ ions Na+ is exchanged with K+ which causes loss of K+. The acetazolamide thus causes loss of Na+, H2CO3– and K+. As a result of this, there is decrease in extracellular fluid base which causes metabolic acidosis. This results in loss of diuretic activity. Hence, acetazolamide is self-limiting diuretic.
(II) Moderately potent diuretics
Benzothiadiazine :
Pharmacological Actions :
Kidney: These drugs prevent reasorbtion of Na+ and Cl– . They are believed to act mainly on the site proximal to Na+ and K+ exchange region in the distal tubules; the glomerular filtration rate is not affected. Initially, the drug causes decrease in Na+ reabsorption in the distalubules and a gradual reduction in extracellur fluid volume. When extracellular fluid volume falls to below normal, the reabsorbtion of Na+ from proximal tubule is stimulated. The amount of Na+ delivered to distal tubule is decreased. This causes decrease in diuretic activity and resistance. Because of strong inhibitory action on Na+ reabsorption a large amount of Na+ is made available to distal segment, where exchange of Kt with Na+ takes place. This results into increased loss of K+ ions.
Metabolic Action: Prolonged use of thiazides cause hyperglycemia and glycosurea. These can aggravate the pre-existing diuretic splliters. The direct inhibition of insulin release and hypocalemia are the possible mechanisms causing hyperglycemia. Thiazides also decreases the excretion of uric acid causing increased uric acid level of blood.
Adverse Reaction :
Hypokalemia and Hypochloremic alkalosis.
Preparation and Doses:
Chlorothiazide – 250 mg tab. 500-1000 mg daily.
Hydrochlorothiazide – 250-500 mg tab. 25-200 mg daily.
Hydroflumethiazide – 50 mg tab. 25-200 mg daily.
Trichloromethazide.
Therapeutic Uses :
As a diuretic in patients with sodium retention oedema.
Clopamide: It is administered in a single daily dose of 20-60 mg in the morning on alternate days. It is well tolerated with a larger duration of action (18-24 hrs.). It does not have any other advantage over thiazide diuretics. Chlorothiaridone and chloroxolone are the other moderately potent thiazides similar to that of thiazide.
(III) Very potent diuretics
Parenteral Organic Mercurial Compounds: Organic mercurial compounds given parenterally are effective diuretics.
Pharmacological Actions :
(1) Kidney: Mercurials acts directly at various sites in the nephron. They inhibit the intracellular enzyme and thus depresses the reabsorption of Na+ and Cl– causing diuresis. Precise mechanism of action is not known. But it is supposed that internal release of divalent mercury ion is responsible for diuretic property. The mercurial ion has affinity for sulphydryl group. It reacts with sulphydryl group of enzymes responsible for tubular reabsorption of Na+. As sulphydryl group from enzymes is made inactive the reabsorption of Na+ decreases causing diuresis. The effect of full dose of mercurial diuresis can be enhanced further by thiazides or aminophylline. Mercurials cause K+ loss as that of thiazides.
(2) Other Action: Mercury is toxic ion and if accumulated in the body is capable of producing mercurial poisoning. These are administered intramuscularly and should never be given intravenously as they may precipitate severe cardiac toxicity. These are rapidly excreted by kidney and the excretion is almost complete by 24 hours.
Adverse Effects :
Intravenous administration causes sudden ventricular fibrillation, collapse, and death. It may also result into renal and hepatic damage. The mercurials cause hypochloremic alkalosis.
Preparations and Doses:
Parenteral mercurial injection contains some amount of theophylline which helps in absorbtion of mercurials and also reduce irritation.
Mersalyl injection I.P. dose 0.5 to 2 ml I.M. on alternate days.
Mercaptomerin sodium injection/thiomerin. dose – 1 ml subcutaneous (S.C.) or intramuscular (I.M.) once or thrice weekly.
Therapeutic Use:
In the treatment of oedema due to nephrosis, and congestive cardiac failure (C.C.F).
Frusemide : It is a potent oral non-mercurial diuretic.
Pharmacological Actions :
(1) Kidney and Electrolytes :
On oral administration the intense diuretic action starts within an hour and is completed in 4-6 hours. It produces more chloride loss than Na+ loss. The frusemide acts along the entire nephron including the loop of Henle with the exception only of distal site where Na+ is exchanged for K+ and H+. Hence, unlike thiazides the urinary excretion of Na+ continues even when patient’s extracellular fluid volume has been severely depleted. In therapeutic doses, it has little effect on carbonic anhydrase. It causes increased excretion of phosphates. Drug enhances Kt excretion and causes little change in urinary pH and its diuretic response is not limited by the state of electrolyte, or acid base balance of the body. The excessive loss of chloride may lead to hypochloremic alkalosis. The K+ loss may cause hypokalemia.
(2) Other Actions:
Like thiazides frusemide can cause increase in blood uric acid level. The administration of drug has been shown to have important peripheral vascular effects leading to pooling of blood in peripheral range. The effect is more important in the treatment of acute left ventricular failure.
Adverse Reaction :
Due to its powerful diuretic nature, frusemide may cause disturbances in electrolyte and water balance of body. Weakness, fatigue and hypotension may also occur. Following IV administration, cardiac arrest may occur. The drug can produce hepatic coma on administration in patients with liver disease. Skin rash, nausea, vomiting and diarrhea are other known adverse reactions.
Preparations and Doses:
Frusemide tab. 40 mg.
Frusemide injection (20 mg in 2 ml) dose – 40 to 100 mg daily depending on severity of oedema.
Therapeutic Use :
Frusemide is an effective and usually safe diuretic. It is more effective in case of severe oedema. When given IV it is most effective in pulmonary oedema. It is also useful for forced diuresis in the treatment of barbiturate poisoning.
Ethacrynic Acid: It is very potent oral diuretic like frusemide.
Pharmacological Actions :
The renal actions of ethacrynic acid are similar to those of frusemide. When given orally the maximum diuresis occur within 2-3 hours while on I.M. administration the effect starts within few minutes. It can cause hypochloremic alkalosis and potassium depletion. Like frusemide, it acts at on various sites of nephron.
Preparations and Doses:
Ethacrynic acid tab. (25 to 50 mg) dose 50-200 mg.
Sodium ethacrynate injection dose 0.5-1 mg/kg body weight. It is more useful in patients with pulmonary oedema.
(IV) Potassium-sparing diuretics
Spironolactone : Spironolactone is an aldoesterone antagonist. It acts by competative antagonism of aldosterone. Thereby, preventing the potassium secretion and decreasing sodium reabsorption. The drug does not produce significant action in normal individuals or in those cases of oedema which are not associated with rise in aldosterone concentration. Drug is given orally in a total daily dose of 100 mg. It has cumulative effect and full response is observed only after few days of therapy.
Adverse Reactions :
No serious toxicity have been reported but it may cause drowsiness and menstrual irregularity. Spironolactone tab. (25 mg), dose 25 mg 2-4 times a day.
Triamterene :
When given orally it increases excretion of water, Na+, Cl– and bicarbonates but it depresses the excretion of K+. It is a weak diuretic when given orally. However, it can enhance action of other diuretics and hence can be combined with other diuretics which causes depletion of K+ to prevent such depletion.
The Important Indication of Diuretic Therapy :
(1) Oedema associated with sodium retention such as cardiac oedema, hepatic and renal oedema.
(2) Pulmonary oedema.
(3) Drug poisoning e.g., salicylate poisoning.
(4) Acute renal failure.
Antidiuretic Agents :
ADH – Antidiuretic hormone: It is released from posterior lobe of pituitary gland, along with oxytocin. The rate of secretion of ADH is mainly dependent on the state of hydration.
Pharmacological Actions :
(1) Kidney: The distal tubule and collecting duct of nephron becomes permeable to water leding to reduction in total urine volume. The absence of ADH causes diabetes insipidus.
(2) Cardiovascular system: In large dose ADH raises blood pressure by direct stimulation of vascular smooth muscles but this is followed by fall in blood pressure due to narrowing of coronary blood vessels and by direct depressant effect of ADH on myocardium.
(3) Other smooth muscles: In large doses it stimulates smooth muscles of gastrointestinal tract causing increase in peristalsis. ADH should not be given by oral route as it is destroyed by trypsin. It is administered by parenteral route. The other antidiuretic drug is chlorpropamide.
You May Read:
