Granulocytes are immune cells that are membrane-bound that function mainly to digest endocytosed particles. This consists of multiple lobes and are thus called polymorphonuclear (PMN) leukocytes. These are white blood cells.
Introduction
- Morphologically, the earliest recognizable granulocytic cells are myeloblasts.
- They are large, open-nuclear chromatin cells.
- Promyelocytes, neutrophil myelocytes, neutrophil metamyelocytes, and neutrophil band cells are called the successive stages through which a myeloblast matures into circulating neutrophil granulocytes.
- In myeloblasts, promyelocytes, and myelocytes, cell division happens, but not usually in metamyelocytes and band cells.
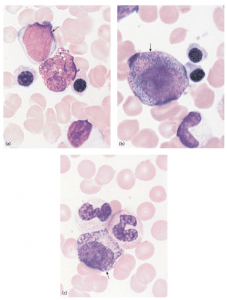
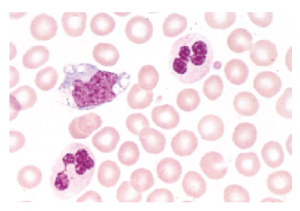
- Three kinds of granulocytes are available: neutrophils, eosinophils, and basophils. The color that the granules stain when treated with a compound dye distinguishes each of these types.
Eosinophils
- Eosinophils represent only a small number of circulating leukocytes(1-6%) and are short-lived cells in circulation with a t1/2 of 8-18 h.
- Normal eosinophil count is less than 500 cells per microliter (cells/mcL).
- Traditionally, eosinophils are known for their role in the fight against parasitic infections and their harmful effects on allergic diseases.
- Eosinophils contribute to stimulating inflammation, which helps to isolate and control a disease site.
- Eosinophils have a similar ability to phagocytose and destroy micro-organisms but are classically associated with the immune response to parasitic infection.
- They are a subset of granulocytes with bright pink granules on hematoxylin and eosin-stained blood films. They are often found in high numbers in allergic and atopic patients.
- For their differentiation from granulocyte precursors, IL-5 signaling appears to be critical.
- In the recruitment and activation of DCs, eosinophils and their active compounds play their role in promoting optimal adaptive immune responses.
Basophils
- Of the granulocytes, basophils are the least common. Less than 3% of your white blood cells account for Basophils.
- There are between 0 and 300 basophils per microliter of blood.
- Basophils are released from the bone marrow as mature cells and then circulate in the blood.
- Cytoplasmic secretory granules containing preformed mediators, including histamine, are circulating cells.
- Basophils are granulocytes that circulate in sites of allergic inflammation and that react to allergic stimuli by migrating.
- Basophils not just act as effector cells but also as promoters of cell differentiation in Th2 play important and nonredundant roles.
- Basophils, including autoimmunity and cancer, are associated with several chronic inflammatory disorders.
- They include very prominent H&E staining cytoplasmic granules that have stores of histamine and heparin as well as proteolytic enzymes.
- They are involved in a variety of immune and inflammatory responses, but in specific reactive conditions, it is unusual to see a marked elevation or depression in their numbers.
Neutrophil
- Neutrophils makeup 55 to 70 percent of your white blood cells and are the most abundant type.
- It is considered to be the first line of defense during inflammation and infections.
- Furthermore, many kinds of tumors are infiltrated with neutrophils. In addition, activated neutrophils release proteinases into the surrounding tissue and damage the host.
- Neutrophils can produce numerous cytokines and chemokines that can influence the ignition and the immune response
- The neutrophil lineage’s maturation process is characterized by a decrease in cell size, along with the acquisition of granules containing agents that are essential for their microbicidal function. The nucleus also starts to adopt its characteristic segmented shape gradually.
- Mature neutrophils have the ability to migrate to areas of inflammation (chemotaxis) where, by interaction with selectins, integrins, and other cell adhesion molecules, they become marginated in the vessel lumen and pass into the tissues.
- Neutrophils are able to phagocytose opsonized microbes once primed by cytokines such as TNFα and IFNγ and destroy them by deploying their intracellular toxic content.
- A substrate for the enzyme myeloperoxidase (MPO), which then produces hypochlorous acid with direct cytotoxic effects, is provided by the release of reactive oxygen species (‘respiratory burst’).
- Neutrophil granules also contain a variety of antimicrobial agents, including defensin, chymotrypsin, and gelatinase.
Granulocytes are important examples of such supplementary cells that can influence dendritic cells’ function significantly. Granulocytes have long been considered exclusively an important player in innate immune responses, but their potential role has been recently acknowledged in contributing to adaptive immune responses. Granulocytes circulating have a comparatively short lifetime of up to a few days. Long life span is nevertheless seen as these cells are easily recruited to infection sites
References
- https://jlb.onlinelibrary.wiley.com/doi/full/10.1189/jlb.4MR0217-048RR
- https://www.sciencedirect.com/topics/medicine-and-dentistry/basophil-cell
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4706937/
