Hemostasis
- It is the instinctive response for the body to stop bleeding and loss of blood.
- Hemostasis occurs when blood is present outside the body or blood vessels.
- Three mechanisms reduce blood loss:
- Vascular spasm: It is the first response as the blood vessels constrict to allow less blood to be lost.
- Platelets plug formation: Platelets stick together to form a temporary seal to cover the break in the vessel wall.
- Blood clotting: Coagulation reinforces the platelet plug with fibrin threads that act as molecular glue.
Vascular Spasm:
- It is the blood vessel’s first response to injury.
- When arteries or arterioles are damaged, the circularly arranged smooth muscle in their walls contracts immediately, a reaction called as vascular spasm.
- The damaged vessels constrict which reduces the amount of blood flow through the area and limits the amount of blood loss.
- This reduces blood loss for several minutes to several hours.
- This response is triggered by factors such as a direct injury to vascular smooth muscle, chemicals released by endothelial cells, and activated platelets and reflexes initiated by local pain receptors.
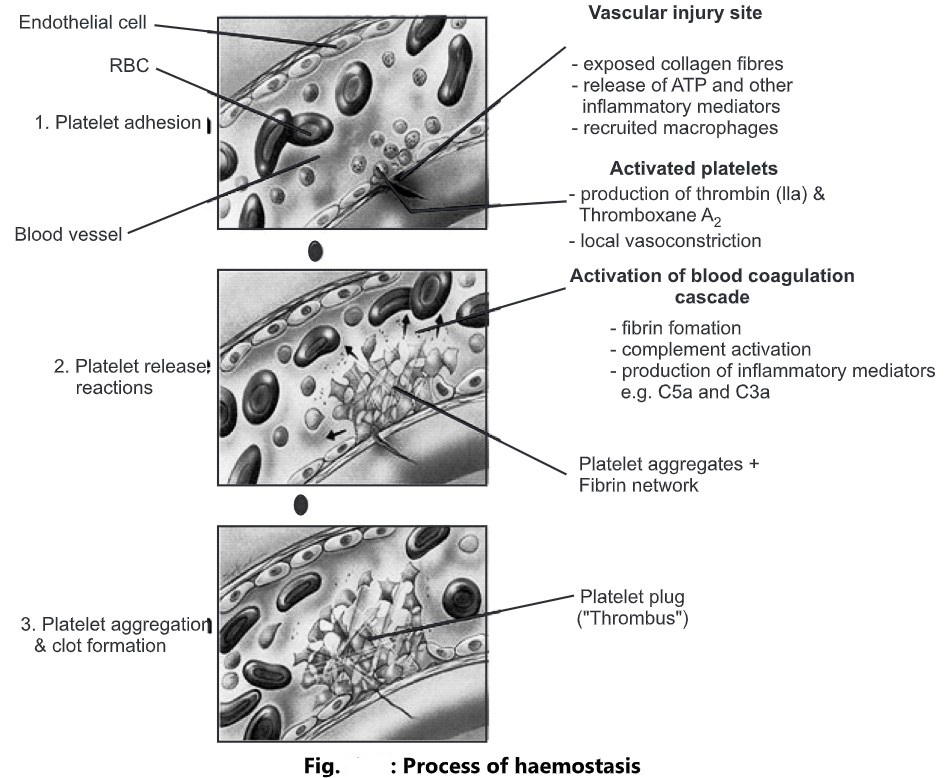
Platelet Plug Formation:
- Platelets play an important role in the hemostatic process.
- Platelets sticks together to form a plug that temporarily seals the break in the vessel wall called as platelet adhesion.
- As they adhere to the collagen fibres of a wound they become spiked and much stickier.
- Then they release chemical messengers such as adenosine diphosphate (ADP), serotonin, and thromboxane A2. This phase is called as platelet release reaction.
- These chemicals are released to cause more platelets to stick to the area and release their contents and enhance vascular spasms. This phase is called as platelet aggregation.
- As more chemicals are released, more platelets stick and release their chemicals; creating a platelet plug.
- Platelets contain Platelet-Derived Growth Factor (PDGF), a hormone that can cause the proliferation of vascular endothelial cells, vascular smooth muscle fibres, and fibroblasts to help repair damaged blood vessel walls.
- The platelet plug formation is activated by a glycoprotein called the Von Willebrand factor (VWF), found in the blood plasma.
- A platelet plug is very effective in preventing blood loss in a small vessel.
Blood Clotting:
- It is the process by which blood forms clots.
- It is a series of chemical reactions that culminates in the formation of fibrin threads.
- It is a complex cascade of enzymatic reactions in which each factor activates many molecules of the next one in a fixed series.
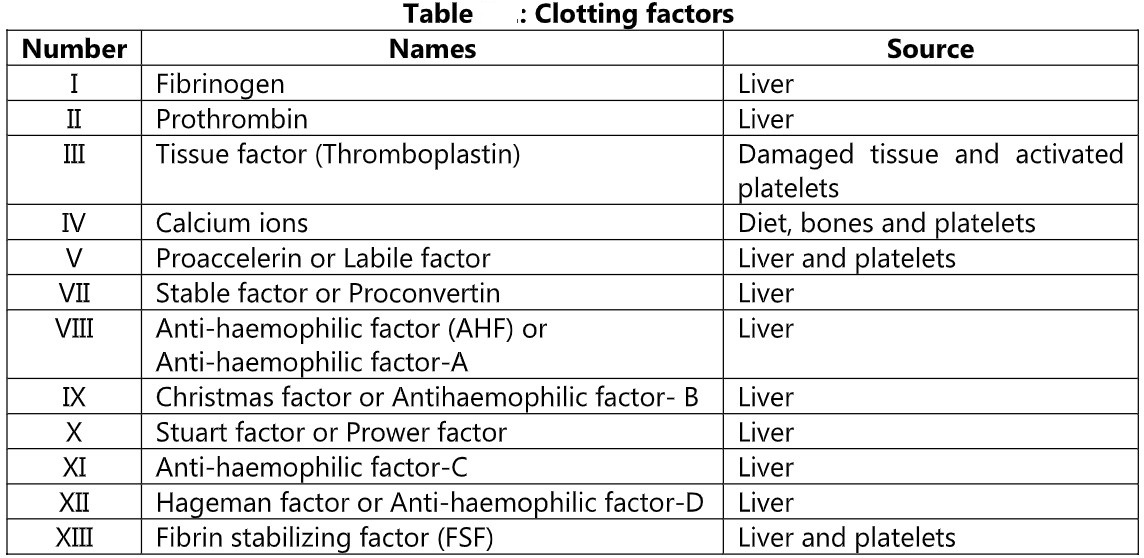
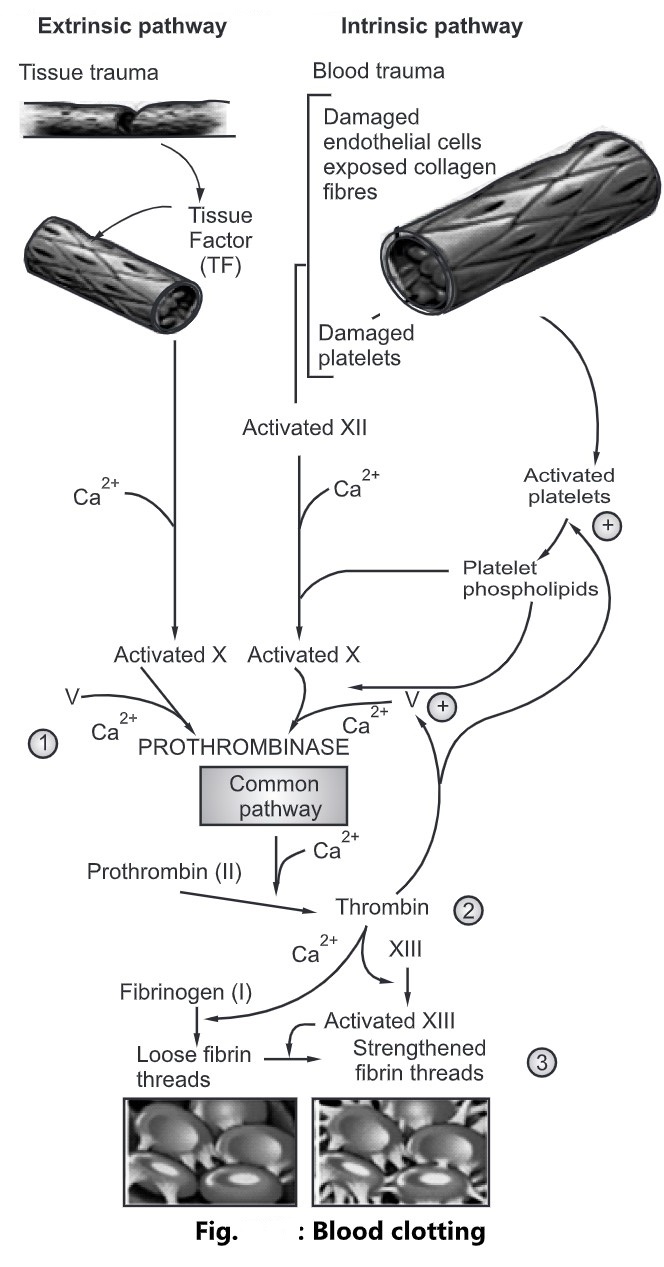
Clotting can be divided into three stages
- Intrinsic pathway: It leads to the formation of prothrombinase with fewer steps which occur rapidly.
- Extrinsic pathway: It leads to the formation of prothrombinase with more number of steps which occur more slowly.
- Common pathway: Once prothrombinase is formed the steps involved in the next two steps of clotting are the same for both the pathways called as common pathways. Prothrombinase converts prothrombin into the enzyme thrombin. Thrombin converts soluble fibrinogen into insoluble fibrin. Fibrin forms the clot.
Extrinsic Pathway:
- It consists of fewer steps and occurs rapidly within a second.
- In this pathway, a tissue protein called as tissue factor (TF) leaks into the blood from cells outside the blood vessels and initiates the formation of prothrombinase.
- TF is a complex mixture of lipoproteins and phospholipids released from the surfaces of damaged cells.
- In the presence of Ca2+, TF activates factor X.
- Once factor X is activated, it combines with factor V, in the presence of Ca2+ to form the active enzyme prothrombinase, completing the extrinsic pathway.
Intrinsic Pathway:
- The pathway is more complex and occurs more slowly, usually in several minutes.
- The activators are either in direct contact with blood or contained within the blood vessel.
- If endothelial cells are damaged, blood comes in direct contact with collagen fibres in the connective tissue around the endothelium of the blood vessel.
- Injury to endothelial cells causes damage to platelets, resulting in the release of phospholipids by the platelets.
- Contact with collagen fibres activates clotting factor XII, which activates clotting factor X.
- Platelet phospholipids and Ca2+, participate in the activation of factor X.
- Once factor X is activated, it combines with factor V to form the active enzyme prothrombinase, completing the intrinsic pathway.
Common Pathway:
- The formation of prothrombinase is the starting point of a common pathway.
- In the second stage of blood clotting, prothrombinase and Ca2+ catalyze the conversion of prothrombin to thrombin.
- In the third stage, thrombin in presence of Ca2+ converts fibrinogen (soluble) to loose fibrin threads (insoluble).
- Thrombin also activates factor XIII (fibrin stabilizing factor), which strengthens and stabilizes the fibrin threads into a sturdy clot.