Hypersensitive Reactions and Its Types
INTRODUCTION
Hypersensitivity is an inflammatory reaction within the humoral or cell-mediated immune response that leads to significant tissue injury, serious disease, or even death. Immediate hypersensitivity is the anaphylactic reaction within the humoral branch which is initiated by antibody/antigen-antibody complexes. They are called so because the symptoms manifest within minutes/hours after a sensitized recipient encounters the antigen. Delayed-type hypersensitivity (DTH) is so-called in recognition of the delay of symptoms until days after exposure.
GELL AND COOMBS CLASSIFICATION
In hypersensitivity reaction, different antibody (Ab) isotypes induce specific immune effector molecules. IgE Ab induces mast cells degranulation with the release of histamine and other biologically active molecules. IgE and IgM Abs induce hypersensitivity reaction by activating complement. Different immune mechanisms give rise to a hypersensitivity reactions. P.G.L Gell and R.R.A Coombs proposed a classification in which hypersensitivity reaction were divided into four types:
Type I Hypersensitivity/Anaphylactic Hypersensitivity
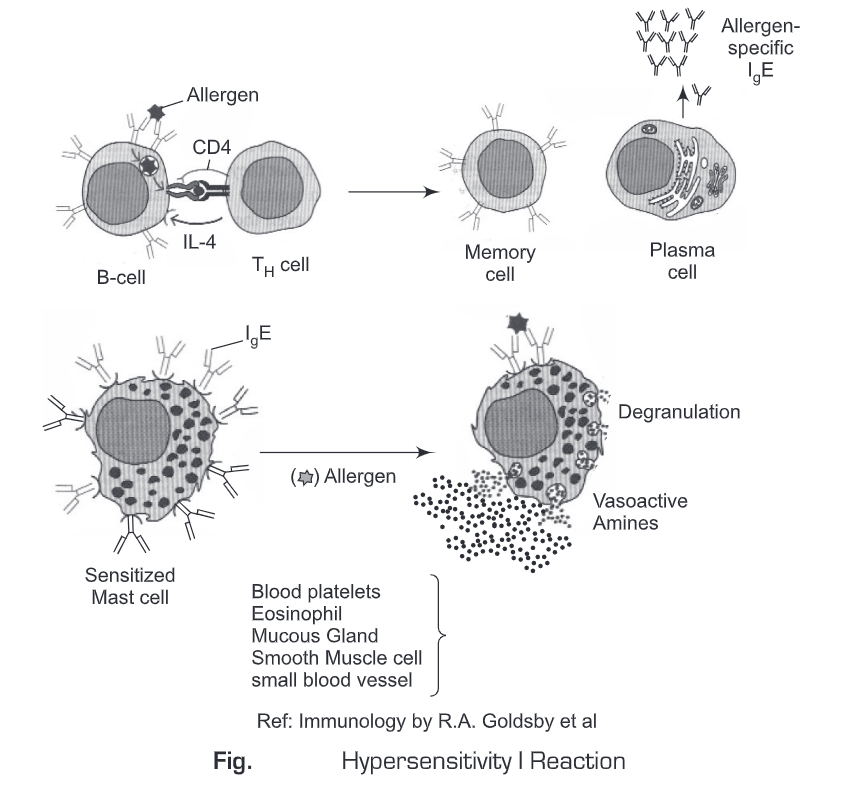
Type 1 hypersensitivity reaction is mediated by IgE. Mast cell or basophil act as primary cellular component of the reaction and the reaction is amplified/or modified by platelets, neutrophils and eosinophils. The reaction can cause a range of symptoms from minor inconvenience to death. The reaction usually takes 15-30 minutes from the time of exposure to the antigen and sometimes delayed to 10-12 hours.
Mechanism: Type 1 hypersensitivity reaction involves production of IgE, in response to certain antigens. Individuals preferentially produce more of TH2 cells that secrete IL-4, IL-5 and IL-13 which in turn favor IgE class switch. IgE has a very high affinity for its receptor (Fcԑ; CD23) on mast cells and basophils. Subsequent exposure to the same allergen results in cross-linking of the cell-bound IgE and triggers the release of various pharmacologically active mediators. Cross-linking of IgE Fc-receptor is important in triggering the mast cells. Degranulation of mast cells is done by increased Ca2+ influx, which is a crucial process. Mast cells may also be triggered by other stimuli such as exercise, emotional stress, chemicals, and anaphylatoxins. These reactions, mediated by agents without IgE-allergen interaction, are not hypersensitivity reactions, although they produce the same symptoms.
Clinical manifestation: Systemic anaphylaxis and localized anaphylaxis such as hay fever, asthma, hives, food allergies, and eczema.
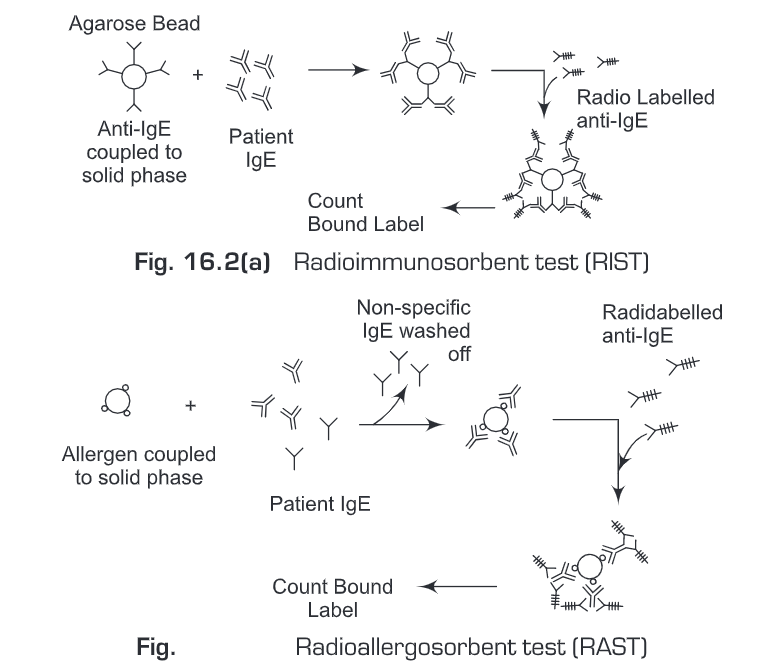
Detection: Type I hypersensitive reactions can be assessed by determining the serum level of total IgE antibody by the radioimmunosorbent test (RIST). RIST can detect nanomolar levels of total IgE. The test serum is reacted with agarose beads coated with rabbit anti-IgE. Then after a washing,125I-labeled rabbit anti- IgE are added. The radioactivity of the beads is measured with a gamma counter and is proportional to the level of IgE in the test serum.
Another similar radioallergosorbent test (RAST) can detect the serum level of IgE specific for a given allergen. The allergen is initially coupled to beads and then the test serum is added. A washing is given to remove any unbound antibody. The amount of specific IgE bound to the solid-phase allergen is then measured by adding ‘I-labeled rabbit anti-IgE, washing the beads, and counting the bound radioactivity.
Treatment
- Symptomatic treatment is done with anti-histamines which block histamine receptors. e.g: Chromolyn sodium and isoproterenol derivatives (Terbutaline, Albuterol).
- Hyposensitization or desensitization is another treatment for a number of allergies, particularly to insect venoms and to some extent pollens.
Type II Hypersensitivity/Cytotoxic Hypersensitivity
Type II hypersensitivity is primarily mediated by antibodies of the IgM or IgG classes and complement. Phagocytes and K cells also play a role. It may affect a variety of organs and tissues. The antigens involved may be endogenous and exogenous chemicals (haptens) which can attach to cell membranes and can cause type II hypersensitivity.
Mechanism: Type II Hypersensitivity reaction occur when Ab reacts with antigenic determinants present on the surface of cells, leading to cell damage or death through complement mediated lysis or antibody-dependent cell-mediated cytotoxicity (ADCC).
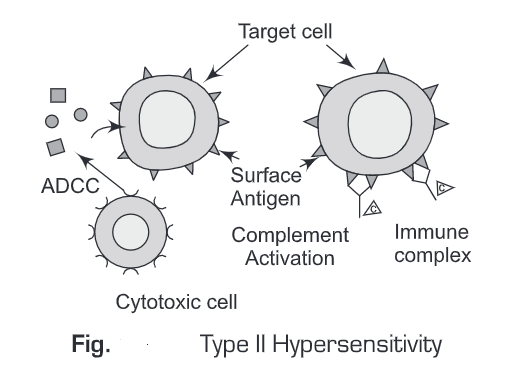
Clinical manifestation: Blood transfusion reaction, erythroblastosis fetalis, autoimmune haemolytic anemia.
Treatment
- Anti-inflammatory and immunosuppressive agents are used to treat Type II hypersensitivity.
Type III Hypersensitivity/Immune Complex Hypersensitivity
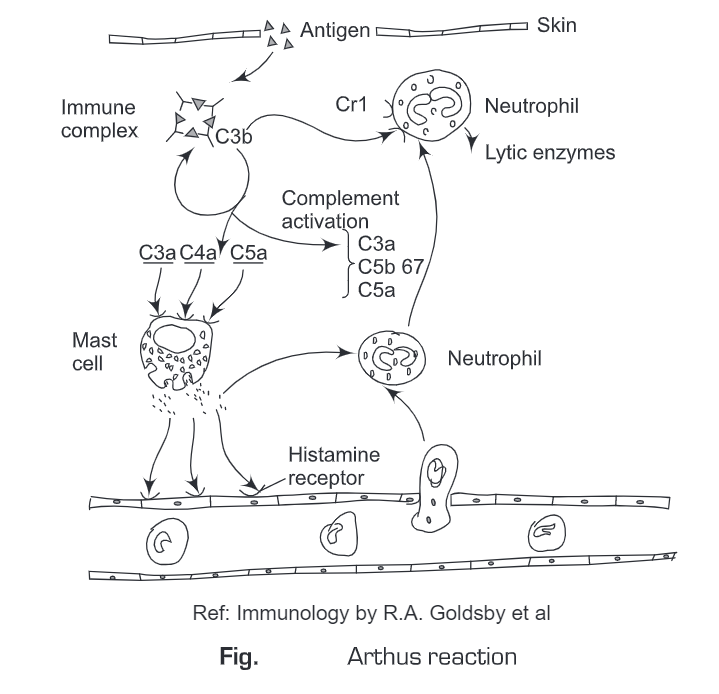
Type III Hypersensitivity is mediated by soluble immune complexes and complement (C3a, 4a, and 5a). They are mostly of the IgG class; sometimes IgM may also be involved. The antigen may be exogenous (chronic bacterial, viral or parasitic infections), or endogenous (non-organ specific autoimmunity). The antigen is soluble and not attached to the organ involved. The damage is caused by platelets and neutrophils. The lesion contains primarily neutrophils, deposits of immune complexes, and complement. Macrophages in later stages of infilteration may be involved in the healing process. The reaction may take 3-10 hours after exposure to the antigen.
Mechanism: It is mediated by the formation of immune complexes and ensuing activation of complement. Complement split product serve as immune effector molecule that elicit localized vasodilation and chemically attract neutrophils. Deposition of immune complexes near antigen entry site can induce an Arthus reaction, by which lytic enzyme released from the accumulated neutrophils and complement membrane attack complex that cause localized tissue damage.
Clinical manifestation: Serum sickness, systemic lupus erythematosus, Arthus reaction, and lupus nehritis.
Treatment: Anti-inflammatory agents are used to treating Type III hypersensitivity.
Type IV Hypersensitivity/Delayed-Type Hypersensitivity
Type IV hypersensitivity is involved in the pathogenesis of many autoimmune and infectious diseases (tuberculosis, leprosy, blastomycosis, histoplasmosis, toxoplasmosis, leishmaniasis, etc.). Type IV hypersensitivity can be classified into three categories depending on the time of onset, clinical and histological presentation.
(a) Contact reaction occurs in 48 -72 hours after the injection of antigen. The antigen may be organic chemicals, poison ivy, or heavy metals and attack the epidermal site. The symptom is characterized by eczema. It involves the lymphocytes, macrophages, and edema of the epidermis.
(b) Tuberculin reaction which peaks 48 hours after the injection of antigen on the intradermal site. The lesion is characterized by induration and erythema. It involves lymphocytes, monocytes, macrophages.
(c) Granuloma reaction occurs due to infections and foreign antigens. It shows the hardening symptom after 21-28 days and involves macrophages, epitheloid, fibrosis, and giant cells.
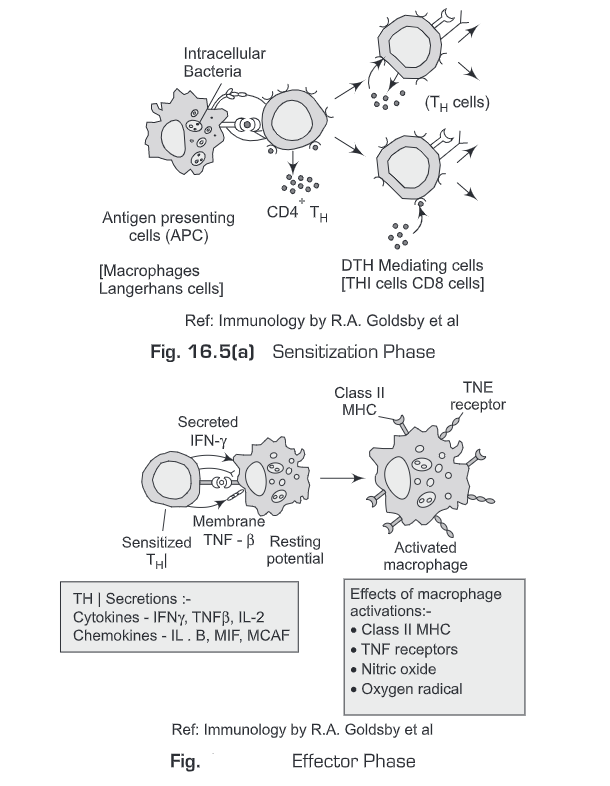
Mechanisms: Delayed hypersensitivity includes T lymphocytes and monocytes/macrophages. Cytotoxic T cells (T) cause direct damage whereas helper T (TH1) cells secrete cytokines which activate cytotoxic T cells and recruit and activate monocytes and macrophages, which cause the bulk of the damage. The delayed hypersensitivity lesions mainly contain monocytes and a few T cells. The DTH response has two phases:
- Sensitization phase — It is the initial phase of 1-2 weeks after primary contact with an antigen. In the sensitization phase, TH, cells get activated and then clonally expand by antigen presented together with the requisite class IT MHC molecule on an appropriate antigen-presenting cell.
- Effector phase— A subsequent exposure to the antigen induces the effector phase of the DTH response. In this phase, T H1 cells secrete a variety of cytokines that recruit and activate macrophages and other nonspecific inflammatory cells.
Clinical manifestation: Autoimmune diseases and graft rejection are in part to delayed hypersensitivity reactions and Insulin dependant diabetes mellitus.
Treatment: Corticosteroids and other immunosuppressive agents are used in treating delayed-type hypersensitivity.