Contents:
- Red blood cells or erythrocytes contain the oxygen-carrying protein hemoglobin that gives the red color to blood.
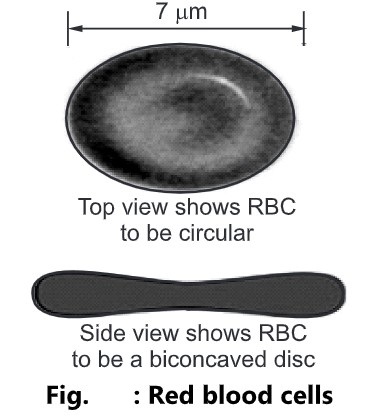
Characteristics of RBCs
- Count: 5.4 million RBCs per microliter (ul) of blood in males and 4.8 million RBCs per µl of blood in females.
- Shape: Biconcave disc-shaped.
- Size: Diameter 7-8 µm and thickness 2 µm.
- Contains Haemoglobin.
-
- It is the iron-containing oxygen transport metalloprotein in the red blood cells.
- It transports oxygen from the lungs to the body tissues.
- When the oxygen concentration is high in the alveoli, the hemoglobin combines with oxygen to form oxyhemoglobin.
- When the blood reaches the tissue with a low concentration of oxygen, the hemoglobin dissociates with the oxygen releasing the oxygen into the body tissues.
- RBCs contain no nucleus, endoplasmic reticulum, ribosomes, and mitochondria.
- RBCs contain a larger surface area because of biconcavity for oxygen diffusion.
- They can easily squeeze through the blood capillaries.
- Their life span is about 120 days.
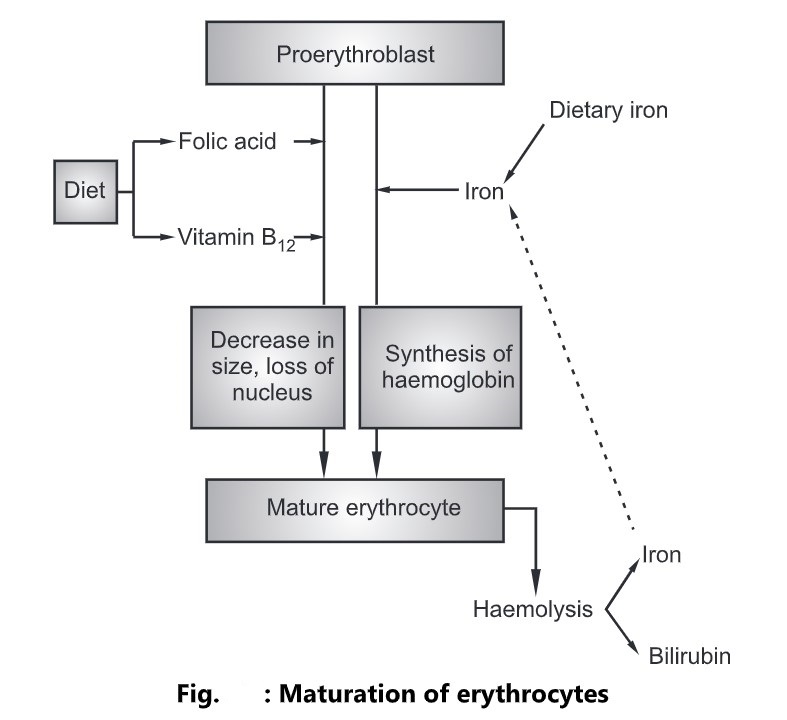
Erythropoiesis
- The process of development of red blood cells from pluripotent stem cells is called erythropoiesis.
- Erythrocytes are produced in the red bone marrow present at the ends of long bones.
- The immature cells are released into the bloodstream as reticulocytes and then mature cells released erythrocytes in one or two days within the circulation.
- During this time they lose their nucleus and therefore become incapable of division.
- The erythropoiesis is characterized by two main features:
- Maturation of cell
- Formation of hemoglobin inside the cell
Maturation of Cell
- During this process, the cell decreases in size and loses its nucleus.
- These changes depend on the presence of vitamin B12 and folic acid.
- These vitamins are present in a normal diet containing dairy products, meat, and green vegetables.
- The absorption of vitamin B12 depends on a glycoprotein called an intrinsic factor secreted by parietal cells in the gastric glands.
- Together they form intrinsic factor-vitamin B12 complex (IF-B12).
- During its passage through the intestine, the bound vitamin is protected from enzymatic digestion and is absorbed in the ileum, a portion of the small intestine.
- Folic acid is absorbed in the duodenum and jejunum where it undergoes change before entering the blood.
- Deficiency of either vitamin B12 or folic acid leads to impaired red cell production.
Formation of Haemoglobin
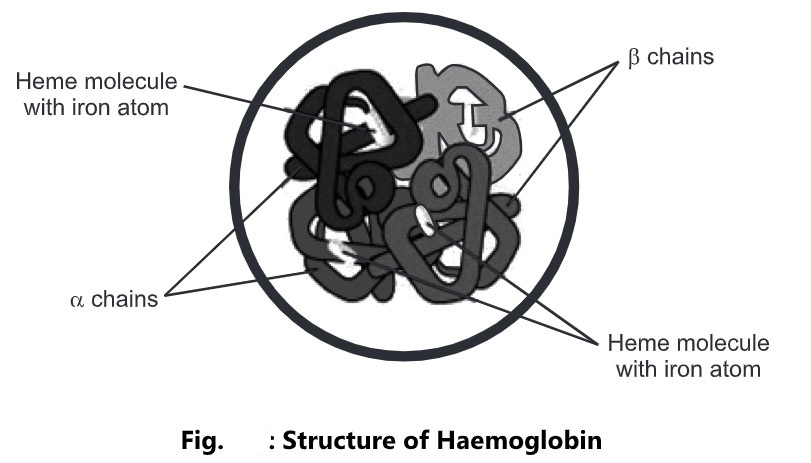
- Hemoglobin is a complex protein, consisting of globin and iron-containing haem, and is synthesized inside the developing erythrocytes in the red bone marrow.
- Hemoglobin in mature erythrocytes combines with oxygen to form oxyhemoglobin, giving blood its characteristic red color.
- Haemoglobin is involved in the transportation of carbon dioxide from the body cells to the lungs for excretion.
- Each hemoglobin molecule contains four atoms of iron.
- Each atom can carry one molecule of oxygen and therefore one hemoglobin molecule can carry up to four molecules of oxygen.
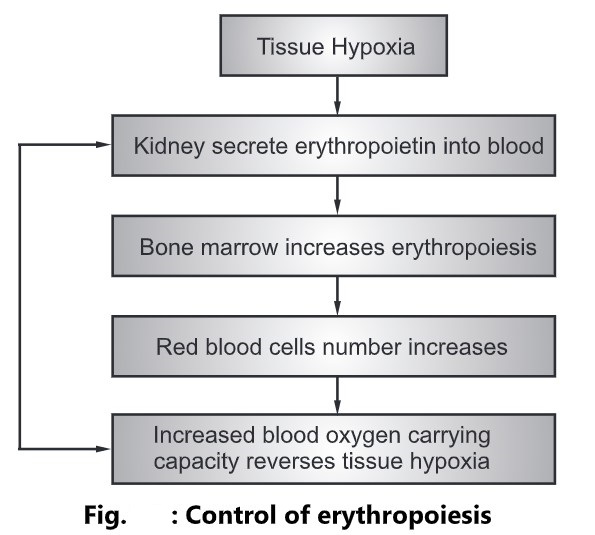
Control of Erythropoiesis
- The number of red cells remains constant, which means that the bone marrow produces erythrocytes at the rate at which they are destroyed.
- This is due to a homeostatic negative feedback mechanism.
- The primary stimulus to increase erythropoiesis is hypoxia, i.e. deficient oxygen supply to the body cells.
- This process occurs when:
-
- The oxygen-carrying capacity of blood is reduced by hemorrhage or excessive erythrocyte breakdown (hemolysis) due to disease.
- The oxygen tension in the air is reduced.
- Hypoxia increases erythrocyte formation by stimulating the production of the erythropoietin hormone by the kidneys.
- Erythropoietin stimulates the production of proerythroblasts and the release of increased numbers of reticulocytes into the blood.
- These changes increase the oxygen-carrying capacity of the blood and reverse tissue hypoxia.
- When the tissue hypoxia is overcome, erythropoietin production gets declines.
- When erythropoietin levels are low, red cell formation does not take place even in the presence of hypoxia, and anemia develops.
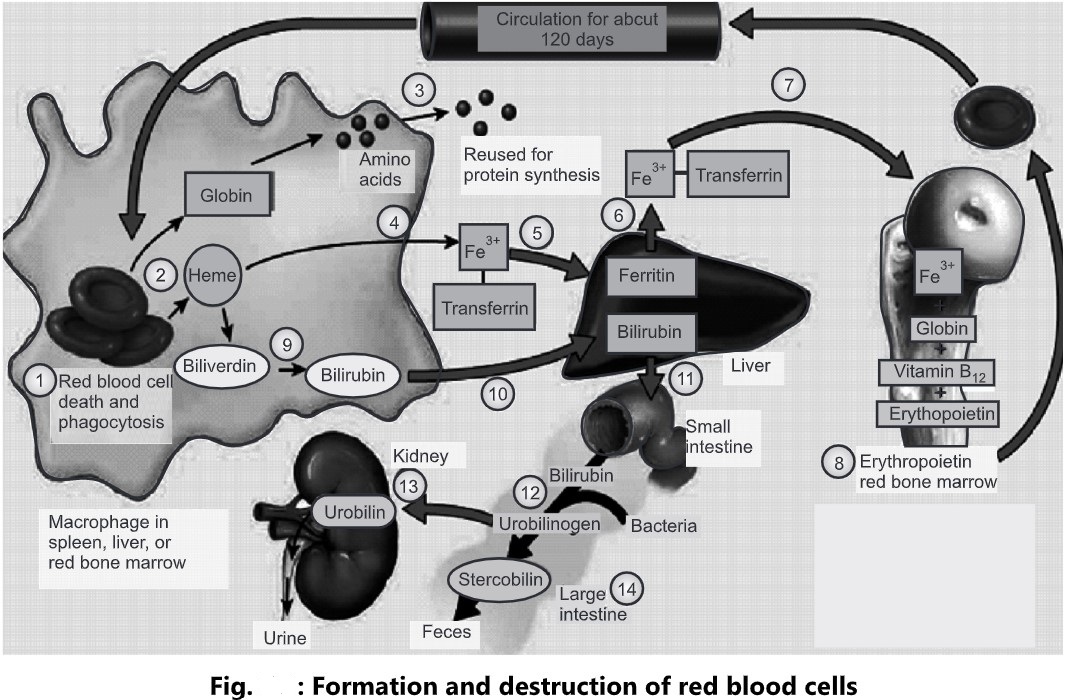
Destruction of Erythrocytes
- The life span of erythrocytes is about 120 days and hemolysis is carried out by phagocytic reticuloendothelial cells.
- The main sites of reticuloendothelial cells are the spleen, bone marrow, and liver.
- As erythrocytes undergo aging, changes in cell membranes make them more susceptible to hemolysis.
- Iron released by hemolysis is retained in the body and reused in the bone marrow to form hemoglobin.
- Biliverdin is formed from the protein part of the erythrocytes.
- It is reduced to the yellow pigment bilirubin and transported to the liver.
- In the liver, it is changed from a fat-soluble to a water-soluble form as a constituent of bile.
- Ruptured red blood cells are removed from circulation and destroyed by fixed phagocytic macrophages in the spleen and liver, and the breakdown products are recycled, as follows;
- Macrophages in the spleen, liver, or red bone marrow phagocytize ruptured and worn-out red blood cells.
- The globin and heme portions of hemoglobin are split apart.
- Globin is broken down into amino acids, that can be reused to synthesize other proteins.
- Iron is removed from the heme portion in the form of Fe3+which associated with the plasma protein transferrin.
- In muscle fibers, liver cells, and macrophages of the spleen and liver, Fe3+ detaches from transferrin and attaches to an iron-storage protein called ferritin.
- Upon release from a storage site or absorption from the gastrointestinal tract, Fe3+ reattaches to transferrin.
- The Fe3+ transferrin complex is then carried to red bone marrow, where RBC precursor cells are used in hemoglobin synthesis. Iron is needed for the heme portion of the hemoglobin molecule, and amino acids are needed for the globin portion. Vitamin B12 is also needed for the synthesis of hemoglobin.
- Erythropoiesis in red bone marrow results in the production of red blood cells, which enter the circulation.
- When iron is removed from heme, the non-iron portion of heme is converted to biliverdin, a green pigment, and then into bilirubin, a yellow-orange pigment.
- Bilirubin enters the blood and is transported to the liver.
- Within the liver, bilirubin is released by liver cells into bile, which passes into the small intestine and then into the large intestine.
- In the large intestine, bacteria convert bilirubin into urobilinogen.
- Some of the urobilinogen is absorbed back into the blood, converted to a yellow pigment called urobilin, and excreted in the urine.
- Most urobilinogen is eliminated in feces in the form of a brown pigment called stercobilin that gives feces its characteristic color.