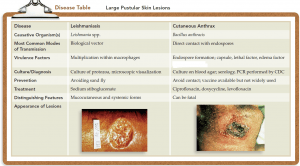
1. Leishmanias
- Leishmaniasis, a zoonosis transmitted among various mammalian hosts by female sand flies. This infection can express itself in several different forms, depending on which species of the protozoan Leishmania is involved.
Cutaneous leishmaniasis
- It is a localized infection of the capillaries of the skin caused by L. tropica, found in Mediterranean, African, and Indian regions.
- A form of mucocutaneous leishmaniasis called espundia is caused by L. brasiliensis, endemic to parts of Central and South America.
- Cutaneous leishmaniasis symptoms: It affects both the skin and mucous membranes. Another form of this infection is systemic leishmaniasis. Leishmania is transmitted to the mammalian host by the sand fly when it ingests the host’s blood.
- The disease is endemic to equatorial regions that provide favorable conditions for the sand fly. Numerous wild and domesticated animals, especially dogs, serve as reservoirs for the protozoan.
- Although humans are usually accidental hosts, the flies freely feed on them. At particular risk are travelers or immigrants who have never had contact with the protozoan and lack specific immunity.
- Leishmania infection begins when an infected fly injects the motile forms of the protozoan into the host while feeding. After being engulfed by macrophages, the parasite converts to a nonmotile reproductive form and multiplies in the macrophage.
- The manifestations of the disease vary with the fate of the macrophages. If they remain fixed, the infection stays localized in the skin or mucous membranes, but if the infected macrophages migrate, systemic disease occurs.
- In cutaneous leishmaniasis, a small red papule occurs at the site of the bite and spreads laterally into a large ulcer. The edges of the ulcer are raised and the base is moist. It can be filled with a serous/purulent exudate or covered with a crust. Satellite lesions may occur.
Mucocutaneous leishmaniasis
- It usually begins with a skin lesion on the head or face and then progresses to single or multiple lesions, usually in the mouth and nose. Lesions can be quite extensive, eventually involving and disfiguring the hard palate, the nasal septum, and the lips.
- There is no vaccine; avoiding the sand fly is the only prevention.
- Mucocutaneous leishmaniasis treatment: The disease can be treated with chemicals such as sodium stibogluconate. Other antimicrobials may be indicated for secondary infections of the lesions.
2.Cutaneous Anthrax
- This form of anthrax is the most common and least dangerous version of infection with Bacillus anthracis.
- The bacteria is a small aerobic or facultatively-anaerobic, gram-positive or gram-variable, encapsulated, spore-forming rod.
- Cutaneous anthrax causes: It is caused by endospores entering the skin through small cuts or abrasions.
- It results from inoculation of B. anthracis spores through the abraded skin into subcutaneous tissues.
- The bacteria subsequently germinate and multiply locally and begin toxin production. This leads to the characteristic edema (most lethal) and cutaneous ulceration.
- Germination and growth of the pathogen in the skin are marked by the production of a papule that becomes increasingly necrotic and later ruptures to form a painless, black eschar (ess′-kar).
- In the fall of 2001, 11 cases of cutaneous anthrax occurred in the United States as a result of bioterrorism (along with 11 cases of inhalational anthrax). Mail workers and others contracted the infection when endospores were sent through the mail.
- The infection can be naturally transmitted by contact with hides of infected animals (especially goats). Left untreated, even the cutaneous form of anthrax is fatal approximately 20% of the time. A vaccine exists but is recommended only for high-risk persons and the military.
- Humans are relatively resistant to cutaneous anthrax but break in the skin can allow the organism to enter the skin and once inside, the organism spreads rapidly and affects the lungs, kidney, spleen and even brain and cause meningitis which is extremely fatal.
- Upon suspicion of cutaneous anthrax, ciprofloxacin, levofloxacin and/or doxycycline should be used initially. If the isolate is found to be sensitive to penicillin, patients can be switched to that drug.
References
