Contents:
Transplantation Immunology
INTRODUCTION
Transplantation: It is an act of transferring cells, tissues, or organs from one site to another. Many diseases can be cured by the implementation of healthy organ tissue or cells (a graft) from one individual (donor) to another in need of transplant (host). Alux Carrel reported the first systemic study of transplantation in 1908, he interchanged both kidneys in series of nine cats. Organs that can be transplanted are the Kidney, heart, liver, pancreas, lungs, thymus, and intestine and tissues include heart valves, bones, tendons, cornea, skin, and veins. The kidneys are the most commonly transplanted organs, followed by the liver and then the heart. A variety of immunosuppressive agents can delay or prevent the rejection of the transplanted organ, e.g. Calcineurin inhibitor, mTOR inhibitor, Anti-proliferative, corticosteroids, and antibodies, etc. Different types of grafts/transplants.
Autograft or Auto-transplantation
Self tissue is transferred from one body site to another in the same individual. In some cases, autograft is done with surplus tissue or tissue that can regenerate, or tissues more desperately needed elsewhere, E.g. transferring healthy skin to burnt area in burnt patients and use of healthy old vessels to replace blocked coronary arteries.
lsograft
It is a kind of allograft in which organ or the tissue is transferred from a donor to a genetically identical recipient. In humans, isograft can be performed in genetically identical individuals (monozygous two). Isografts are separated from other types of transplants because they are anatomically identical to allografts, but do not trigger an immune response.
Allograft or Allo-transplantation
Allograft is a transplant of an organ or tissue between genetically different markers of the same species. Most human tissue and organ transplants are allografts. The recipient’s immune system will identify the organ as foreign due to genetic differences between the organ and the recipient and attempt to destroy it, causing transplant rejection.
Xenograft or Xeno-transplantation (Greatest Rejection)
A transfer of organ or tissue between different species. For example, Graft of Baboon heart into a human. Xenotransplantation is often an extremely dangerous and serious type of transplant due to the increased risk of non-compatibility, rejection, and disease carried in the tissue.
IMMUNOLOGIC BASIS OF GRAFT REJECTION
Allograft Rejections Display Specificity and Memory
In allograft rejection, T-cells play a major role. Old grafts and MHC antigens are responsible for the most intense graft rejection. Tissues that are antigenetically similar are said to be histocompatible. They do not produce an immunological response that leads to tissue rejection. The various antigens that determine histocompatibility are encoded by more than 40 different loci, but loci responsible for the most vigorous rejection reactions are located within MHC. The organization of MHC is called H-complex in mice and HLA complex in humans. Various tissue typing procedures are used to screen potential donors and recipients.
Initially, they are screened for ABO blood group compatibility
↓
Blood group antigens are expressed on RBC’s epithelial cells and endothelial cells.
↓
Ab produced in the recipient against any of these Ag’s present on transplant tissues.
↓
Induced Ab mediated complement lysis of the incompetitive donor cells.
Microtoxicity Tests
These tests are used for HLA typing of potential donor and recipient. HLA is based on Ab-mediated microcytotoxicity used to indicate the presence or absence of various MHC alleles.
Procedure
WBC’s are potential donor and recipient and are distributed into the series of wells on a microtitre plate.
↓
Abs specific for Class I and Class II MHC alleles are added to different wells.
↓
Complement is added to wells and cytotoxicity is accessed by the uptake or exclusion of various dyes by the cells.
↓
WBC’s express MHC allele for which a particular monoclonal antibody is specific, then the cells will be lysed on the addition of complement and these dead cells will take up a dye such as trypan blue.
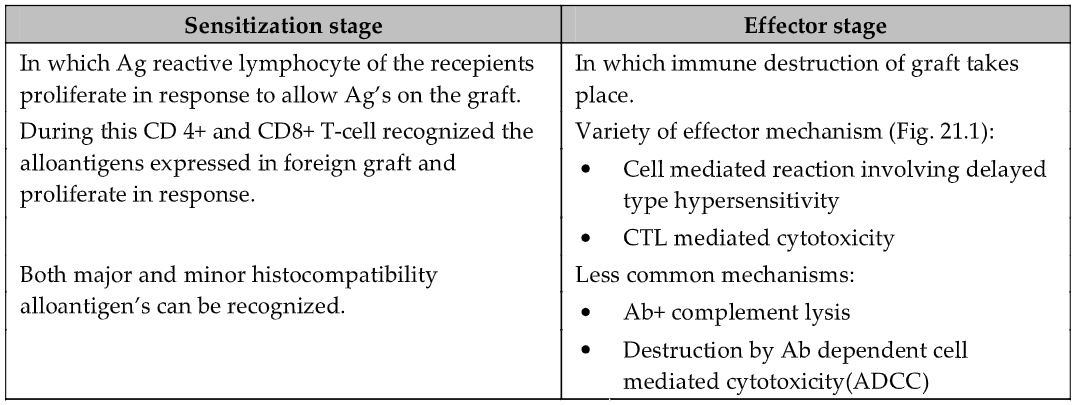
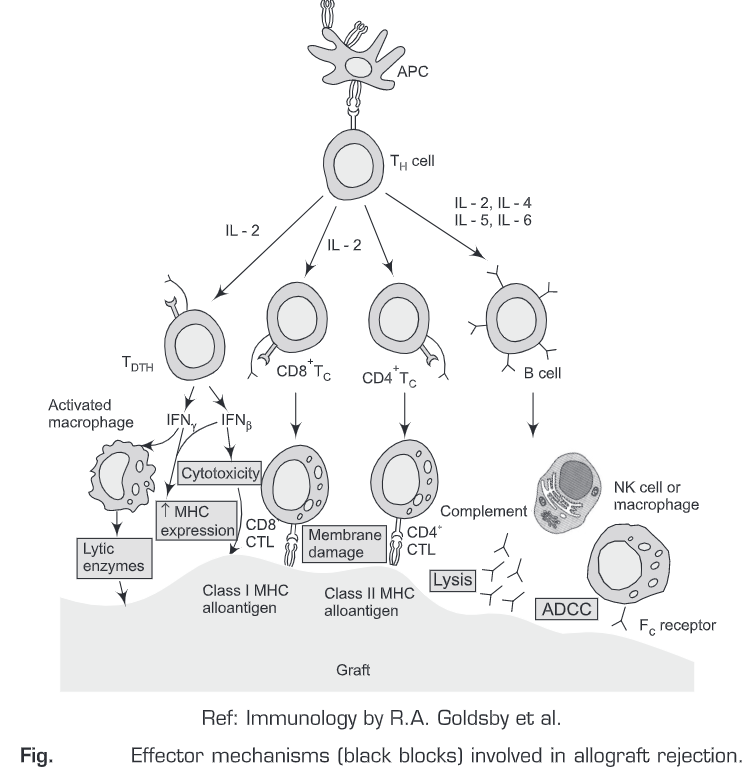
Stages of Graft Rejection
Graft rejection is caused principally by the cell-mediated immune response to alloantigens (MHC molecules).
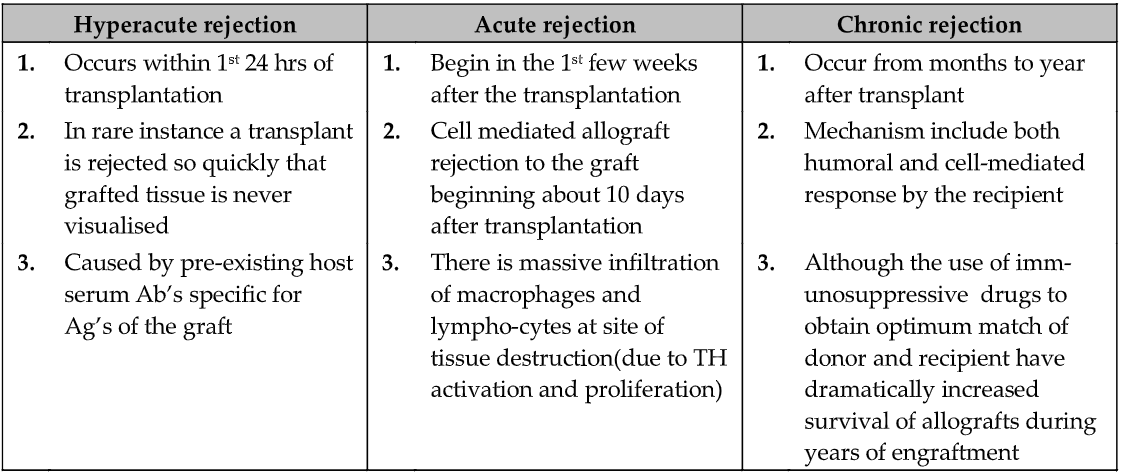
CLINICAL MANIFESTATION OF GRAFT REJECTION
Graft rejection has various time courses.
- Depending on the type of tissue or organ group.
- The immune response is involved.
CLINICAL TRANSPLANTATION
For a number of illnesses, a transplant is the only means of therapy. For example, transplanted organs are the heart, kidney, pancreas, lung, skin, etc. Immunosuppressive drugs greatly increase the short-term survival of transplant but medical problems arise from using these drugs and chronic rejection prevail. Factors responsible for which an organ is transplanted depends on:
- The clinical situation in which transplantation is indicated
- Availability of tissue or organ
- The difficulty of performing transplantation and caring for the post-transplantation patients.
Heart Transplantation
Heart transplantations are used to remove a damaged or diseased heart and replaces it with a healthy one. A healthy heart comes from a donor who has died. Heart transplants are now the third most common organ transplant operation in the U.S. Doctors may recommend a heart transplant for heart failure caused by: Coronary artery disease, Cardiomyopathy (disease of the heart muscle), Heart valve disease, and multiple congenital heart defects in babies.
Kidney Transplantation
A kidney transplant is an operation that replaces a diseased or damaged kidney from the body. The transplanted kidney takes over the work of the two kidneys that failed. During a transplant, the surgeon places the new kidney in the recipient’s lower abdomen and connects the artery and vein of the new kidney to the recipient’s artery and vein. Often, the transplanted kidney will start making urine as soon as recipient blood starts flowing through it. But sometimes it takes a few weeks to start working. Many transplanted kidneys come from donors who have died. Some come from a living family member. The wait for a new kidney can belong. An immunosuppressant is usually required to prevent transplant rejection.
Liver Transplantation
Liver transplantation removes the diseased liver and replaces it with a healthy one. Most transplant livers come from a donor who has died. Sometimes a healthy person donates part of his or her liver for a specific patient. In this case, the donor is called a living donor. The most common reason for transplantation in adults is cirrhosis (healthy liver cells are killed and replaced with scar tissue) and in children is biliary atresia (a disease of the bile ducts).
Lung Transplantation
Lung transplantation is surgery to replace one or both diseased lungs with healthy lungs. During the operation, the surgeon makes a cut in the chest and removes the diseased lung. The surgeon then sews the new lung to the main blood vessels and air passage. Lung transplantation is recommended if the disease cannot be controlled by any other way. These diseases include COPD (chronic obstructive pulmonary disease), cystic fibrosis, diopathic pulmonary fibrosis interstitial lung disease, Primary pulmonary hypertension. Complications of lung transplantation include rejection of the transplanted lung and infection.
Pancreas Transplantation
A pancreas transplant is a surgery to place a healthy pancreas from a donor into a person with a diseased pancreas. A common reason for this type of damage is diabetes. Pancreas transplants can enable people with type I diabetes to give up insulin shots. An experimental procedure called islet cell transplantation transplants only the parts of the pancreas that make insulin. Immuno-suppressant is usually required to prevent transplant rejection.
Skin Transplantation
It is the replacement of damaged or burnt skin in patients with a new skin of donors. Skin Transplantation is usually done to treat burn victims. An immunosuppressant is usually required to prevent transplant rejection.
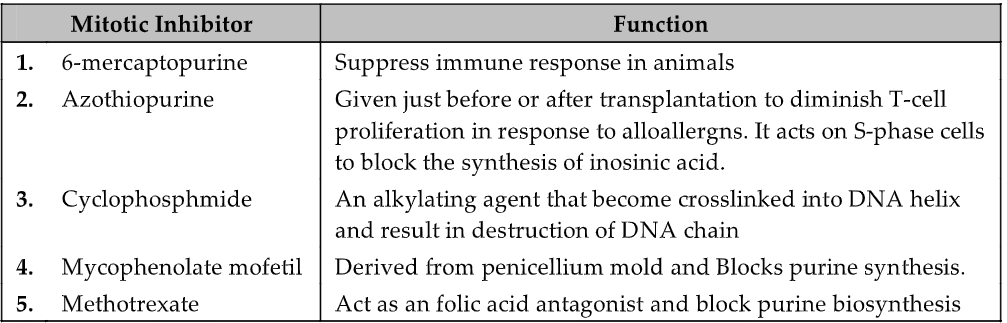
GENERAL IMMUNOSUPPRESSIVE THERAPY
Allogenic transplantation requires some degree of immuno-suppression if the transplant is to survive. The disadvantage of most immunosuppressive treatments is that they are non-specific and result in generalized immunosuppression of response of all allergens. The patient on long-term immunosuppressive therapy is at high risk of hypertension, cancer and metabolic bone disease.
- Mitotic inhibitors thwart T-cell proliferation
- Corticosteroids: e.g., prednisone and dexamethasone are anti-inflammatory agents and are often given to transplant recipient with other immunosuppressents to prevent acute episode of graft rejection.
- Fungal metabolites: Many fungal metabolites are immunosuppressant. e.g., Cyclosporin A and FK 506 block the activation of resting T-cells by inhibiting the transcription of genes encoding IL2 and IL-2 receptors. Ripamycin-immunophillin complex block proliferation and differentiation of activate TH cells. Due to profound properties of these agents, they are used in transplantation of heart, liver, kidney and bone marrow.
- Total lymphoid irradiation eliminates lymphocytes. X radiation can be used to eliminate lymphocyte in transplant recipient just before grafting because lymphocytes are extremely sensitive to X-rays.
SPECIFIC IMMUNOSUPPRESSIVE THERAPY
Experimental approaches using monoclonal antibodies offer the possibility of specific immunosuppression. These antibodies may act by:
(a) Deleting the population of reactive cells—The use of antibodies directed against various surface molecules on the cells of immune system can successfully suppress T-cell activity. Depletion of T-cells to suppress graft rejection involves the use of monoclonal antibody to CD3 molecules of TCR complex. Injection of these antibodies causes rapid depletion of mature T-cells. The depletion is caused by the binding of AB coating T-cells to Fc receptor on phagocytic cells, which then phagocytose and deplete T-cells. In another example, Graft survival can be increased by using monoclonal antibodies specific for high-affinity IL-2 receptor. As IL-2 receptor expressed only on activated T-cells, exposed to Anti-CD 25 after graft specifically block proliferation of T-cells activated in response to alloantigens of graft. Difficulty with the using antibodies to prolong graft survival in human is that they are generally of non human origin.
(b) Inhibiting co-stimulatory signals leading to anergy in specifically reactive cells—T-cells activation requires interaction of TCR with its ligand and reaction of co-stimulatory receptors with their ligands. Contact between one of the co-stimulatory receptors CD28 on the T-cell and its ligand, B7 on APC, is blocked by reaction of B7 with soluble ligand CTLA-4lg. CTLA-4 is coupled to an IgH chain, which slows its clearance from the circulation. This process specifically suppresses graft rejection without inhibiting the immune response to other antigens.
Questions
- Define transplantation. When was the first transplantation done, by whom and in which organ?
- What are the different types of transplants/grafts?
- Discuss the immunologic basis of graft rejection.
- What is microtoxicity test?
- What are the different stages of graft rejection?
- Discuss the clinical manifestations of graft rejection.
- Differentiate between hyperacute, acute and chronic rejections.
- Discuss in brief the clinical transplantations.
- Write short note on general and specific immunosuppressive therapy.
