Contents:
Introduction
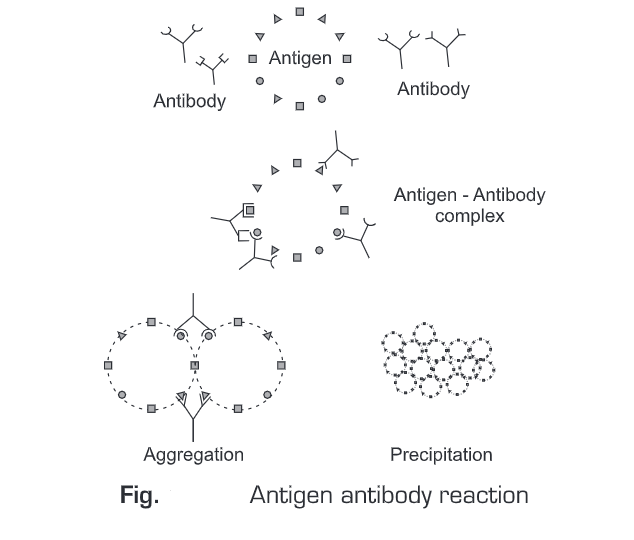
- Antigen antibody reactions occur when an antigen combines with a corresponding antibody to produce an immune complex.
- Therefore, an antigen-antibody reaction is thus a bimolecular association which is similar to an enzyme-substrate interaction but the only difference is that antigen-antibody reaction does not lead to irreversible chemical interaction.
- The basis for antigen-antibody reactions is the non-covalent interactions like hydrogen bonds, ionic bonds, van der Waal interactions, hydrophobic interactions, etc.
- These interactions are individually weak, therefore, a large number of such interactions work together in an antigen-antibody reaction.
- The in vitro study of antigen-antibody reactions is known as serology. The principle for all diagnostic immunological tests is serological reactions.
- The binding of an antibody with an antigen of the type that stimulated the formation of the antibody results in agglutination, precipitation, complement fixation, greater susceptibility to ingestion and destruction by phagocytes, or neutralization of an exotoxin.
- The main use of antigen-antibody reactions is in the determination of blood groups for transfusion, serological ascertainment of exposure to infectious agents, and the development of immunoassays for the quantification of various substances. Schematically an Antigen-Antibody- Reaction can be represented as:
Ag + Ab —> [Ag-Ab] —> Aggregation —> Precipitation/ Agglutination/ Neutralization
For diagnostic immunological tests, the serological tests must possess high specificity and sensitivity. Specificity is the ability of an antibody to recognize a single specific antigen. There is a high degree of specificity in antigen-antibody reactions. Antibodies can distinguish differences in
- primary structure of an antigen,
- isomeric forms of an antigen, and
- the secondary and tertiary structure of an antigen.
Therefore specificity implies that:
- Antibody is specific for a single and specific antigen
- Antibody will not cross-react with other antigens
- It will not give false-positive results
Sensitivity means the lowest amount of antigen that can be detected. If in a diagnostic test an antibody is capable of detecting a single antigen molecule, then such a test possesses the highest sensitivity. The amount of antigen detected in a test is directly proportional to the amount of antibody used. Enzyme-Linked ImmunoSorbent Assays (ELISA) are the most sensitive serological tests.
TYPES OF ANTIGEN-ANTIBODY REACTION
Antigen-antibody reactions are of three types depending upon the type of the complex formed. These are:
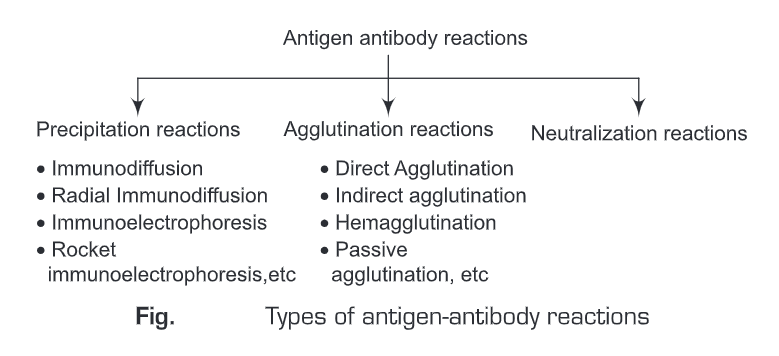
Precipitation Reaction
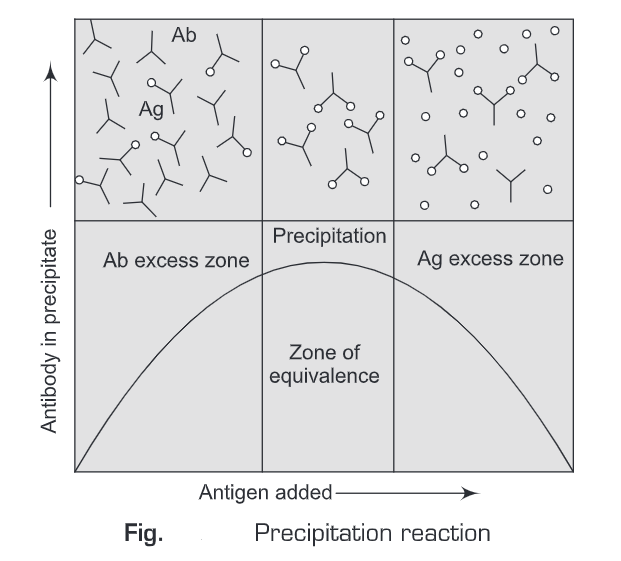
- When a soluble antibody (IgM or IgG) interacts with a soluble antigen and results in the formation of an insoluble (visible) complex (precipitate), it is known as a precipitation reaction.
- Precipitation reactions depend on the formation of lattices. Both antigen and antibody should be present in optimal concentrations for precipitation to occur.
- Excess of either the antigen or antibody may decrease the lattice formation and simultaneously precipitation.
- When the antigen-antibody ratio is optimal, maximum precipitation will occur and this is known as the zone of equivalence.
- From the curve shown in Figure below, it is clear that when the antibody is in excess, it will be present in the supernatant as an unreacted antibody in the form of a soluble complex of antigen such that one molecule of antigen is bound by many antibody molecules.
- And if the antigen molecules are in excess, they will also be found in the supernatant with one /two molecules of antigen bound to a single antibody molecule.
- Soluble antigen-antibody complex is formed within minutes but visible precipitate formation takes a longer time.
- Precipitation reactions may take one or two days to complete. Antibodies that interact with antigens and result in the formation of precipitates are called precipitins.
- Precipitation reactions can be easily observed in vitro, therefore they play an important role in serological tests.
- If the precipitation reactions are carried out in agarose gel, they are known as immuno-diffusion tests.
- Antigen-antibody specificity can be studied using these immunodiffusion tests. The precipitation reactions carried in agarose gel can be studied by immuno-diffusion or Ouchterlony method, radial immuno-diffusion or Mancini method, immunoelectrophoresis, rocket immuno- electrophoresis or Laurel method, countercurrent immuno-electrophoresis, etc.
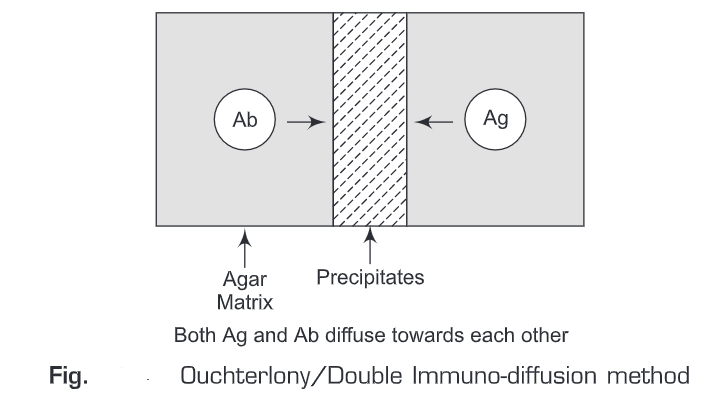
- Immuno-diffusion—Immuno-diffusion is also known as Ouchterlony method (technique). Principle of immuno-diffusion method is the diffusion of antigen and antibody radially from the wells towards each other along the concentration gradient. When the concentration of antigen and antibody molecules is equal, a precipitin band (white) appears at the junction of antigen-antibody complex. Precipitin bands are of three types depending on the type of epitopes. These are:
(a) Line of identity: If the antigens have identical epitopes against a single antibody.
(b) Line of partial identity: If the antigen have some identical epitopes but one unique also.
(c) Line of nonidentity: If unrelated antigens are present and they don’t have identical epitopes.
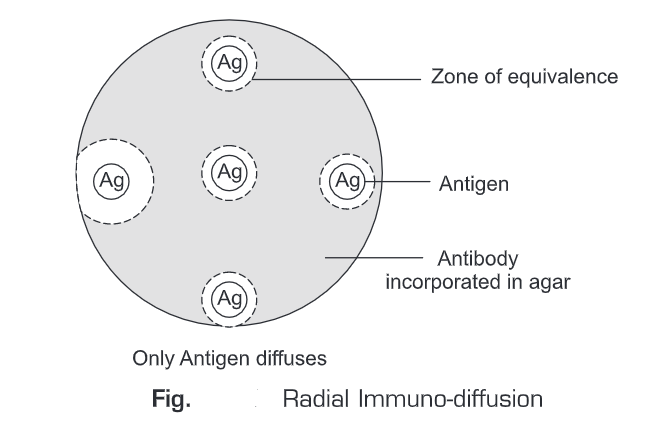
- Radial Immuno-diffusion—Radial immuno-diffusion is also known as Mancini method. In this method the gel is initially punched off and then the antigen and antibody molecules are incorporated into the gel. If suitable antibody dilution is present in the gel, the antigen will diffuse through the gel and when the equivalence region is reached, a precipitate ring is formed around the well. Concentration of the antigen is proportional to the diameter of the precipitin ring.
Agglutination Reactions
- The word agglutination is derived from the latin word agglutinare, meaning “to glue to.” When a particular antigen interacts with an antibody specific for that particular antigen and results in the formation of visible clumps, it is known as agglutination reaction.
- The antibody responsible for the agglutination reaction is known as agglutinin. Similar to precipitation reactions, excess of antibody or antigens also inhibit the agglutination reactions. This mechanism of agglutination inhibition is known as the prozone effect.
- Agglutination tests are 100 times more sensitive than precipitation tests. Agglutination tests are specific, rapid, inexpensive, and sensitive.
- Agglutination is used in many clinical tests to determine the antibody titer of sera or to identify bacteria.
- For example, mixing serum with a culture of Salmonella typhi can confirm the diagnosis of typhoid fever.
- If the serum contains antibody to S. typhi, the bacteria will clump, otherwise, no clump formation takes place. Agglutination reactions are further of the following types:
- Direct Agglutination—When a soluble antibody interacts with an insoluble antigen (antigen on insoluble particle or on the cell surface) and results in clumping is known as direct agglutination. Direct agglutination reactions are used to test the patient’s serum against large, cellular antigens to screen for the presence of antibodies. Direct agglutination reactions can also be used to determine antibody titer.
- Indirect Agglutination—To test the patient’s serum for the presence of antibodies against soluble antigens serum is mixed with latex spheres with the soluble antigens attached. Such antibodies then lead to visible agglutination of the latex spheres with the soluble antigens attached. Alternatively, antibodies may be attached to the latex spheres to test for the presence of soluble antigens in patient serum.
- Hemagglutination—Hemagglutination reactions involve red blood cells agglutination reactions. Hemagglutination reactions are used in blood typing, diagnosis of certain diseases, and the identification of viruses. Viral hemagglutination occurs when spikes on the virus cause agglutination of red blood cells – there is no antigen-antibody interaction. Probably the most familiar use of agglutination is blood typing and is called hemagglutination. Erythrocytes are mixed with antibodies directed against specific blood group antigens such as the major antigens A, B, and D (Rh). Transfusion reactions occur when recipient blood contains antibodies against donor antigens. Agglutination occurring in the vascular system of the recipient could lead to the blockage of vessels and death. Typing involves mixing a sample of blood separately with three antibodies, anti-A, anti-B, and anti-D. If the antigen is present in the blood sample, the red blood cells will agglutinate and form visible clumps. For example, if the blood type is type A, antigens are present and will agglutinate with anti-A. Similarly, if B antigens are present, erythrocytes will clump when exposed to anti-B. If neither antigen is present on the red blood cells in the sample, no agglutination will occur on exposure to anti-A or anti-B, and the sample is blood type O. In addition, some individuals have an additional antigen on their red blood cells called D or Rhesus (Rh) antigen. Cells containing this antigen, so-called Rh-positive cells, will agglutinate due to Anti-D.
- Leukoagglutination—Leukoagglutination is white blood cells agglutination reactions. For example PH-L form of phytohaemagglutinin.
- Passive agglutination—Passive agglutination is a further refinement of haemagglutination. In passive agglutination reactions, the soluble antigens or antibodies are adsorbed on inert particulate surface or chemically coupled to cells; or insoluble particles such as charcoal particles or latex beads. Passive agglutination reactions are five times more sensitive than direct agglutination reactions. Passive agglutination is commonly used in rapid diagnostic tests. Latex agglutination tests are widely used for detection of specific serum antibodies for rheumatoid arthritis or Staphylococcus aureus, etc. In rheumatoid arthritis, the patient makes an antibody (mainly IgM) to his own IgG. The latex particles are coated with IgG and mixed with the patient’s serum. Agglutination indicates a positive test.
Neutralization Reactions
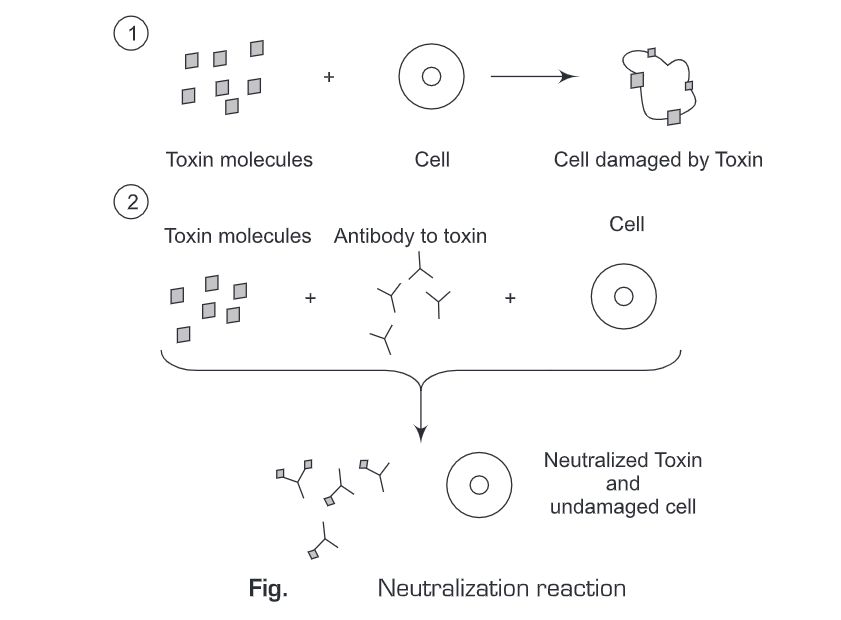
- Neutralization reactions involve the interaction of an antibody with an antigen such that the antigen is blocked or distorted to eliminate its biological activity.
- In neutralization reactions, the harmful effects of a bacterial exotoxin or virus are eliminated by a specific antibody.
- An antitoxin is an antibody produced in response to a bacterial exotoxin or a toxoid that neutralizes the exotoxin.
- In a virus neutralization test, the presence of antibodies against a virus can be detected by the antibodies’ ability to prevent cytopathic effects of viruses in cell cultures.
- Antibodies against certain viruses can be detected by their ability to interfere with viral hemagglutination in viral hemagglutination inhibition tests.
- Neutralization reactions can occur in vitro as well as in vivo. For example,
- Effect of a toxin on a susceptible cell and neutralization of the toxin by antitoxin.
- Viral haemagglutination test to detect antibodies to a virus. Such viruses lead to haemagglutination with the RBCs under normal situations. But if antibodies against the virus are present, they neutralize and inhibit the haemagglutination process.