Excretory Products and their eliminations
- Animals accumulate ammonia, urea, uric acid, carbon dioxide, water and ions like Na+, K+, Cl–, phosphate, sulphate, etc., either by metabolic activities or by other means like excess ingestion.
- These substances have to be removed totally or partially. In this chapter, you will learn the mechanisms of elimination of these substances with special emphasis on common nitrogenous wastes.
- Ammonia, urea and uric acid are the major forms of nitrogenous wastes excreted by the animals.
- Ammonia is the most toxic form and requires a large amount of water for its elimination, whereas uric acid, being the least toxic, can be removed with a minimum loss of water.
- The process of removal of metabolic wastes from the body is called excretion.
Osmoregulation
- The regulation of solute movement and hence water movement (which follows solutes by osmosis) is called osmoregulation. Maintenance of saltwater concentration in steady state.
On the basis of osmoregulation, animals are either osmoconformers or osmoregulators.
(1) Osmoconformers
These animals can not actively control the osmotic condition of their body fluids. Instead of this, they change or adapt the osmolarity of body fluids according to the osmolarity of the surrounding medium
Eg. All marine invertebrates and some fresh water invertebrates.
(2) Osmoregulators
- These animals maintain an intemal osmolarity different from the surrounding medium in which they inhabit.
- Osmoregulator animals must either eliminate excess water if they are in hypotonic medium or they should continuously take in water to compensate for water loss if they are in hypertonic medium.Due to this the osmoregulator animals have to spend energy
Eg. Most vertebrates. except hagfish
| Characters | Types Of Animals | ||
| Ammonotelic | Ureotelic | Uricotelic | |
| Excretory matter | Ammonia | Urea | Uric acid |
| Requirement of water | Very large | Less than ammonia | Least |
| Mechanism of Excretion | By diffusion across body surfaces or through gill surfaces(in fish) as the ammonium ion | Ammonia produced y metabolism is converted into urea in the liver and released into the blood which is filtered and excreted out y the kidneys. | In the form of paste or pellet |
| Toxicity | highest | Less than ammonia | Least |
| Examples | Teleosts(much bony fish) Aquatic insects, Aquatic amphibia | Mammals, Marine fishes, Amphibia (frog) | Birds, insects land snails, many reptiles |
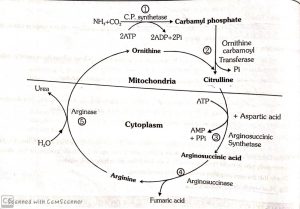
- Urea is produced in the liver by the urea cycle or ornithine cycle.
Ornithine cycle
- In this cycle, 2 molecules of NH₃, 1 molecule of CO₂, 3 ATP molecules are consumed in urea formation.
EXCRETORY ORGANS IN ANIMALS
| Excretory organs | Protonephridia (Flame cells) | Nephridia | Malpighian | Green glands or Antennal glands | Kidneys |
| Examples | Ø Platyhelminthes Ø Rotifers Ø Cephalochordate Ø Some annelids | Annelids (Earthworm) | Most of the insects | Crustaceans (Prawns) | All vertebrates |
HUMAN EXCRETORY SYSTEM
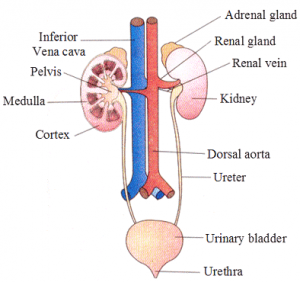
- In human’s, the excretory system consists of a pair of kidneys, one pair of ureters, a urinary bladder and urethra.
Kidneys
- Shape and Size: Kidneys are reddish-brown, bean-shaped structures situated between the levels of last thoracic and third lumbar vertebra close to the dorsal inner wall of the abdominal cavity.
- Each kidney of an adult human measures 10-12 cm in length, 5-7 cm in width, 2-3 cm in thickness with an average weight of 120-170 g.
- The left kidney is a little higher than the right one because of more space being occupied by the liver on the right side. So, only in human beings, the right kidney is slightly below the left.
- But in other mammals, e.g., rabbit, the left kidney is below the right.
- Towards the centre of the inner concave surface of the kidney is a notch called hilum through which ureter, blood vessels and nerves enter.
Kidney is covered by 3 protective layers which are as follows:
1.Renal Capsule : It is innermost, tough protective cover made up of white fibrous connective tissue,with few elastic fibres and few muscles.
2.Adipose Capsule : It is the middle cover involving adipose tissue and acts as shock absorber.
3.Renal Fascia : It is the outermost fibrous cover linking it with the abdominal wall.
As the kidneys are fused with the body wall on the dorsal side, peritoneal cover is present only on the
ventral side. This arrangement is called retroperitoneal arrangement.
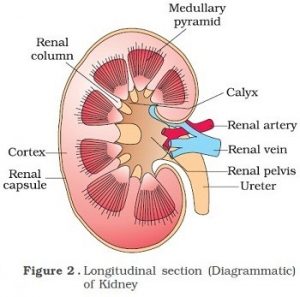
Internal structure of Kidney
- Inner to the hilum is a broad funnel-shaped space called the renal pelvis with projections called calyces.
- The outer layer of kidney is a tough capsule.
- Inside the kidney, there are two zones, an outer cortex and an inner medulla.
- The medulla is divided into a few conical masses (medullary pyramids) projecting into the calyces (sing. : calyx).
- The cortex extends in between the medullary pyramids as renal columns called Columns of Bertini
- Each renal pyramid has a broad base towards the cortical side.
- Apex is pointed and is called renal papilla
- 1-3 renal papillae project into a cavity called minor calyx, which join up and form major calyces
- Interstitial fluid of medulla region has a higher osmotic concentration equal to some 1200 mOsm/L. due to higher quantity of two solutes, NaCl and urea.
- Cortical region close to medulla is called juxtamedullary area.
- The major calyces open into a broad funnel-shaped structure called renal pelvis placed inner to hilum.
- It is lined by transitional epithelium. It leads into ureter.
URETER
- Urine passes from the pelvis into the ureter. Both the ureters open through separate oblique openings into the urinary bladder.
- The obliquity of the openings prevent the backflow of urine.
URINARY BLADDER
- Externally, the bladder is lined by involuntary muscle while internally the bladder is lined by transitional epithelium or urothelium.
- This epithelium has great capacity to expand so that large volume of urine can be stored.
- Opening of urinary bladder is controlled by sphincters made of circular muscles.
- In human two sphincters are present.
Inner = Internal sphincter (made up of involuntary muscle)
Outer = Extemal sphincter (Voluntary muscle).
- These normally remain contracted and during micturition these relax to release urine.
URETHRA
- Urinary bladder opens into a membranous duct called Urethra.
- The urethra leads to end of the penis in males and into the vulva in females.
NEPHRONS
- Nephrons is the structural and functional unit of kidney.
- Each nephron consists of two parts- the glomerulus and the renal tubule.
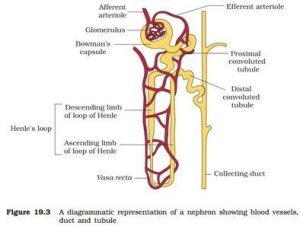
- Glomerulus
- It is a tuft of capillaries formed by the branching of afferent arteriole which is a fine branch of renal artery.
- Glomerular capillaries join to form efferent arteriole.
- Renal tubule
- It begins with Bowman’s capsule which encloses glomerulus.
Bowman’s Capsule
- It is blind double-walled cup-shaped structure. The two walls of Bowman’s capsule are inner visceral and outer parietal. Both are single-layered and are supported over basement membrane.
- Visceral layer (inner wall)
It consists of flat squamous epithelial cells on the periphery and specialised podocytes in the remaining part.
- Parietal layer (outer wall)
It consists of flat squamous epithelium. The space between the two layers of Bowman’s capsule is called lumen or capsular space.
Malpighian body (renal corpuscle)
- Glomerulus along with Bowman’s capsule is called Malpighian body or renal corpuscle.
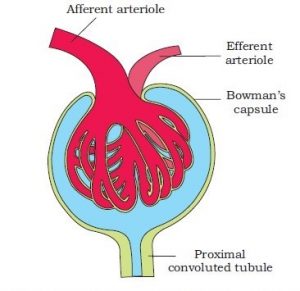
Proximal Convoluted Tubule (PCT)
- Lower part of Bowman’s capsule leads into PCT. The latter is present in the cortex.
- It is highly coiled and surrounded by peritubular blood capillaries.
- PCT is lined by cuboidal epithelium having brush borders with long microvilli for increasing absorptive area.
Loop of Henle
- It is hair-pin loop like tubular part of nephron which descends into renal medulla.
- Loop of Henle is made of two parallel limbs joined by curved base. There is a descending limb and an ascending limb.
Distal Convoluted Tubule (DCT)
- The ascending limb of Henle’s loop continues as DCT.
- DCT is highly coiled part of nephron and lies close to Malpighian body.
Collecting ducts
- The DCTS of many nephrons open into a straight tube called collecting duct, many of which converge and open into the renal pelvis through medullary pyramids in the calyces.
- Collecting ducts enter medulla and form ducts of Bellini.
Vasa recta
- The efferent arteriole emerging from the glomerulus forms a fine capillary network around the renal tubule called peritubular capillaries.
- A minute vessel of this network runs parallel to the Henle’s loop forming a U-shaped vasa recta.
- Vasa recta is absent or highly reduced in cortical nephrons
Types of Nephron
| Cortical Nephron | Juxtamedullary nephrons |
| Constitute of 85% of total | Constitute of 15% of total |
| Malphigian corpusules are located close to the kidney surface | Malphigian corpusules are located at the junction of cortex and medulla |
| Their loop of henle are mostly confined to cortex and a very small part of it runs in the medulla | The loop of henle of these nephrons are long, dipping deep down into the medulla |
| Peritubular capillary network is present | Peritubular capillary network is nnot well developed |
| Vasa recta is absent | Vasa recta is present |
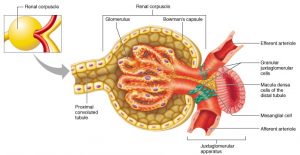
Juxtaglomerular apparatus (JGA)
- The epithelial cells of the distal convoluted tubule that come in contact with the afferent and efferent arterioles are more dense than the other tubular cells and are collectively called the macula densa.
- Along side the macula densa, the wall of afferent arteriole contains modified smooth muscle fibres called juxtaglomerular cells (JG cells) .
- Together with macula densa, they constitute the juxtaglomerular apparatus (JGA).
- Juxtaglomerular cells release renin which helps in regulation of blood pressure and glomerular filtration rate (GFR).
URINE FORMATION
- It involves three main processes namely, glomerular filtration, reabsorption and secretion, that takes place in different parts of the nephron.
Glomerular Filtration
- The first step in urine formation is the filtration of blood, which is carried out by the glomerulus and is called glomerular filtration.
- On an average 1100-1200 mL of blood is filtered by the kidneys per minute which constitute roughly 1/5th of the blood pumped out by each ventricle of the heart in a minute.
- The glomerular capillary blood pressure causes filtration of blood through three layers, ie.,
(i)The endothelium of glomerular blood vessels,
(ii)The epithelium of Bowman’s capsule, and
(iii)A basement membrane between these two layers.
These three structures form the filtration membrane.
- The epithelial cells of Bowman’s capsule called podocytes are arranged in an intricate manner so as to leave some minute spaces called filtration slits or slit pores
- Blood is filtered so finely through these membranes, that almost all the constituents of the plasma except the proteins pass into the lumen of the Bowman’s capsule. Therefore, it is considered as a process of ultrafiltration
- The amount of the filtrate formed by the kidney per minute is called glomerular filtration rate (GFR) which in a healthy individual is approximately 125 ml/min ie.180 litres per day,
- On an average 1100-1200 ml of blood is filtered by kidney per minute (Renal blood flow) which constituteroughly 20-25% of the blood pumped by each ventricle of the heart in a minute (cardiac oútput) and of this blood about 650 ml is the blood plasma (55%). This 650 ml is called Renal plasma flow (RPF). About 20%of the blood plasma filtered by all nephrons of both kidney in a minute. It is 125 ml which called glomerular filtration rate (GFR).
Filtration fraction = GFR/RPF
= 125/650 ml/min
= 1/5
- The kidneys have built-in mechanisms for the regulation of glomerular filtration rate.
- One such efficient mechanism is carried out by juxta glomerular apparatus (JGA). JGA is a special sensitive region formed by cellular modifications in the distal convoluted tubule and the afferent arteriole at the location of their contact.
- A fall in GFR can activate the JG cells to release renin which can stimulate the glomerular blood flow and thereby the GFR back to normal.
Reabsorption
- A comparison of the volume of the filtrate formed per day (180 litres per day) with that of the urine released (1.5 litres), suggest that nearly 99 per cent of the filtrate has to be reabsorbed by the renal tubules. This process is called reabsorption.
- The tubular epithelial cells in different segments of nephron perform this either by active or passive mechanisms.
- For example, substances like glucose, amino acids, Na+ , etc., in the filtrate are reabsorbed actively whereas the nitrogenous wastes are absorbed by passive transport.
- Reabsorption of water also occurs passively in the initial segments of the nephron
Tubular secretion
- During urine formation, the tubular cells secrete substances like H+, K+ and ammonia into the filtrate.
- Tubular secretion is also an important step in urine formation as it helps in the maintenance of ionic and acid base balance of body fluids
FUNCTIONS OF THE TUBULES
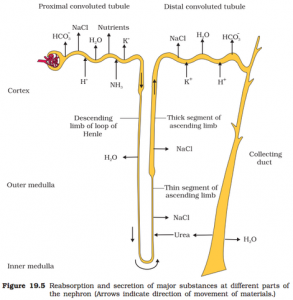
Proximal convoluted tubule (PCT)
- It is lined by simple cuboidal brush border epithelium which increases the surface area for reabsorption.
- Nearly,all of the essential nutrients, and 70-80% of electrolytes and water are reabsorbed by this segment.
- PCT also helps to maintain the pH and ionic balance of the body fluids by selective secretion of hydrogen ions and ammonia into the filtrate and by absorption of HCO3-, from it.
Loop of Henle
- Reabsorption is minimum in ascending limb of loop of Henle.
- However, this region plays a significant role in the maintenance of high osmolarity of medullary interstitial fluid.
- The descending limb of loop of Henle is permeable to water but almost impermeable to electrolytes. This concentrates the filtrate as it moves down.
- The ascending limb is impermeable to water but allows transport of electrolyte actively or passively.
- Therefore,as the concentrated filtrate pass upward, it gets diluted due to the passage of electrolytes to the medullary fluid.
Distal convoluted tubule (DCT)
- Conditional reabsorption of Na+ and water takes place in this segment.
- DCT is also capable of reabsorption of HCO³, and selective secretion of hydrogen and potassium ions and NH₃, to maintain the pH and sodium-potassium balance in blood.
Collecting duct
- This long duct extends from the cortex of the kidney to the inner parts of the medulla.
- Large amounts of water could be reabsorbed from this region to produce a concentrated urine.
- This segment allows passage of small amounts of urea into the medullary interstitium to keep up the osmolarity.
- It also plays a role in the maintenance of pH and ionic balance of blood by the selective secretion of H⁺ and K⁺ ions
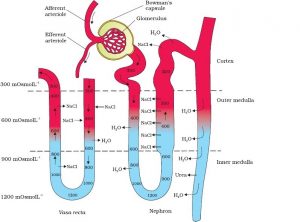
MECHANISM OF CONCENTRATION OF THE FILTRATE
(Counter current mechanism)
- Mammals have the ability to produce a concentrated urine. The Henle’s loop and vasa recta play a significant role in this.
- The flow of filtrate in the two limbs of Henle’s loop is in opposite directions and thus forms a counter current.
- The flow of blood through the two limbs of vasa recta is also in a counter current pattern.
- The interstitial fluid of the kidney increases in osmolarity from 300 to 1200 mOsmol L⁻1 from the centre to the inner medulla.
- This gradient is mainly caused by NaCl & Urea.
- Loop of Henle maintains the interstitial gradient of NaCl.
- NaCl is transported by the ascending limb of Henle’s loop which is exchanged with the descending limb of vasa recta.
- NaCl is returned to the interstitium by ascending part of vasa recta.
- The second solute urea is added to the interstitial medullary fluid in small amount by diffusing out of the collecting duct.
- Urea remaining in the collecting duct is eventually excreted out.
- Urea reenters in the ascending thin segment of the loop of Henle by diffusion.
- This special arrangement of Henle’s loop and vasa recta is called the counter current mechanism. This mechanism helps to maintain a concentration gradient in the medullary interstitium.
- Presence of such interstitial gradient helps in an easy passage of water from collecting tubule.
- As the filtrate flow down in the collecting tubule more and more water moves out of the tubule by osmosis which makes filtrate hypertonic to blood.
- Human kidney can produce urine nearly four times concentrated than the initial filtrate.
REGULATION OF KIDNEY FUNCTION
- Control by Antidiuretic Hormone (ADH)
- Osmoreceptors in the body are activated by changes in blood volume, body fluid volume and ionic concentration.
- An excessive loss of fluid from the body can activate these receptors which stimulate the hypothalamus to release antidiuretic hormone (ADH) vesopressin from the neurohypophysis.
- ADH facilitates water reabsorption from latter parts of the tubule thereby preventing diuresis.
- An increase in body fluid volume can switch off the osmoreceptors and suppress the ADH release to complete the feedback.
- ADH can also affect the kidney function by constrictory effects on blood vessels.
- This causes an increase in blood pressure. An increase in blood pressure can increase the glomerular blood flow and thereby the GFR.
- In this situation, the osmoreceptor cells also promote thirst. Drinking reduces the osmolarity of the blood, which inhibits the secretion of ADH, thereby completing the feedback circuit.
- Control by Juxtaglomerular Apparatus (JGA)
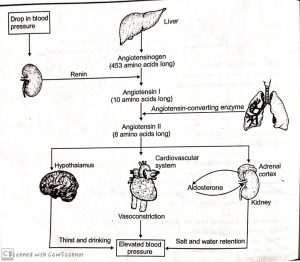
- JGA operates a multi-hormonal Renin Angiotensin-Aldosterone System (RAAS).
- Whenever there is a fall in Glomerular blood flow Glomerular blood pressure/GFR can activate J.G. cells to release an enzyme called renin, into the blood stream.
- In the blood, renin initiates chemical reactions that convert a plasma protein, called angiotensinogen to a peptide, called angiotension II, which works as a hormone.
- Angiotensin II being a powerful vasoconstrictor, increases the glomerular blood pressure and thereby GFR.
- It also increasesblood volume in two ways.
- Firstly, by signaling the distal part of nephron reabsorb more NaCl and water
- Secondly, by stimulating the adrenal gland to release aldosterone, a hormone that induces the distal convoluted tubule to reabsorb more Na⁺ and water. This leads to an increase in blood volume and pressure, completing the feedback circuit by supporting the release of renin.
Atrial Natriuretic Factor (ANF) : (Antagonistic to RAAS)
- When BP or blood volume rise, the wall of atria of the heart stretch and release ANF.
- ANF cause vasodilation (dilation of blood vessels) and thereby decrease the blood pressure.
- ANF also inhibits the release of renin from the kidney and check on the renin-angiotensin mechanism.
MICTURITION
- Urine formed by the nephron is ultimately carried to the urinary bladder where it is stored till a voluntary signal is given by the central nervous system (CNS).
- This signal is initiated by the stretching of the urinary bladder as it gets filled with urine.
- In response, the stretch receptors on the walls of the bladder send signals to the CNS.
- The CNS passes on motor messages to initiate the contraction of smooth muscles of the bladder and simultaneous relaxation of the urethral sphincter causing the release of urine.
- The process of release of urine is called micturition and the neural mechanisms causing it is called the micturition reflex.
- Urine : An adult human excretes, on an average, 1 to 1.5 litres of urine per day. The urine formed is a light yellow-coloured watery fluid which is slightly acidic (pH – 6.0) and has a characteristic odour.
- On an average, 25-30 g of urea is excreted out per day. Various conditions can affect the characteristics of urine.
- Analysis of mine helps in clinical diagnosis of many metabolic disorders as well as malfunctioning of the kidney. For example, presence of glucose (glycosuria) and ketone bodies (ketonuria) in urine are indicative of diabetes mellitus.
- Diabetes mellitus is caused by the hyposecretion (less secretion) of insulin hormone which is secreted from the endocrine part of the pancreas.
Abnormal Constituents in Urine
- Protein (albumin) during injury to renal tract, Glomerulonephritis
- Bile salts and pigments – during jaundice
- Glucose during diabetes mellitus
- Ketone bodies (acetoacetic acid, B-hydroxybutyric acid) – during diabetes mellitus, prolonged fasting.
- Creatinine – Hyperthyroidism, Starvation
ROLE OF OTHER ORGANS IN EXCRETION
Other than the kidneys, lungs. liver and skin also help in the elimination of excretory wastes.
Lungs
- Our lungs remove large amounts of C02 (200 ml/min) and also significant quantities of water every day in normal resting condition.
- Water loss via lungs is small in a hot humid climate and large in cold dry climates.
Liver
- The liver is the largest gland of our body.
- It is the main site for the elimination of cholesterol, bile pigments (bilirubin and biliverdin), degraded steroid hormones, some vitamins and many drugs.
- The liver secretes these substances in the bile. Bile, in turn, carries these materials to the intestine, which are ultimately eliminated with the faeces.
Skin
- The sweat and sebaceous glands in the skin can eliminate certain substances through their secretions, i.e., sweat and sebum respectively.
- The sweat produced by sweat glands is a watery fluid containing NaCl, small amounts of urea and amino acids and glucose etc.
- Though the primary function of sweat is to facilitate a cooling effect on the body surface, it also helps in the removal of some of the wastes mentioned above.
- Sebaceous glands eliminate certain substances like sterols, hydrocarbons through sebum.
- Sebum is a waxy protective secretion which provides a protective oily covering for the skin.
DISORDERS OF THE EXCRETORY SYSTEM
- Malfunctioning of kidneys can lead to accumulation of urea in blood, a condition called uremia, which is highly harmful and may lead to kidney failure. In such patients, urea can be removed by a process called Hemodialysis
- During the process of haemodialysis, the blood drained from a convenient artery is pumped into a dialysing unit called an artificial kidney.
- Blood drained from a convenient artery is pumped into a dialysing unit after adding an anticoagulant like heparin.
- The unit contains a coiled cellophane tube surrounded by a fluid (dialysing fluid) having the same composition as that of plasma except for the nitrogenous wastes.
- The porous cellophane membrane of the tube allows the passage of molecules based on the concentration gradient.
- As nitrogenous wastes are absent in the dialysing fluid, these substances freely move out, thereby clearing the blood.
- The cleared blood is pumped back to the body through a vein after adding anti-heparin to it. This method is a boon for thousands of uremic patients all over the world.
Kidney transplantation is the ultimate method in the correction of acute renal failures (kidney failure).
- A functioning kidney is used in transplantation from a donor, preferably a close relative, to minimise its chances of rejection by the immune system of the host.
- Modern clinical procedures have increased the success rate of such a complicated technique.
Renal calculi: Stone or insoluble mass of crystallised salts (oxalates, etc.) formed within the kidney.
Glomerulonephritis: Inflammation of glomeruli of the kidney.
