HIV/AIDS: Structure and Properties
AIDS- Acquired Human immunodeficiency virus is an immunoregulatory condition that is often fatal because it predisposes the person to serious opportunistic or potentially neoplasmic infections. This is caused by the loss of helper T cells due to HIV infection (human immunodeficiency virus).
Structure and Properties of HIV
- It is part of the Lentivirus subgroup of the family Retroviridae. HIV is a retrovirus with RNA.
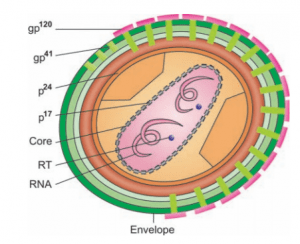
- The cylindrical nucleoid in the mature virion is the special morphologic characteristic of HIV.
- In electron micrographs, the diagnostic bar-shaped nucleoid can be observed. It shows the hallmark exotic flower appearance under the electron microscope.
- In 1984, Dr. Rober C. Gallo discovered HIV.
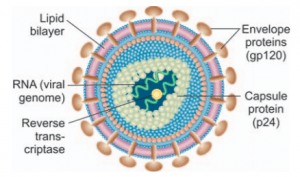
- The virus comprises three genes, gag, pol, and env, necessary for a replicating retrovirus.
- The virus has a glycoprotein-rich outermost envelope (gp41, gp120, gp160) and a two-component protein inner heart, whereas the reverse transcriptase enzyme capable of retrograde transcription of viral RNA into viral DNA has a special characteristic.
- The main proteins, the surface proteins, and the regulatory proteins (p31, p66) are genetically regulated by the respective gag, env and pol loci.
- The env locus is subject to regular genetic alteration among the three inbuilt control mechanisms, leading to a change in the virus’ antigenic structure.
- In addition following 5 genes code for polypeptides are identified as under:
TAT (transactivation gene)
REF (regulator of virus gene) May be involved in regulation of HIV expression
NEF (negative factor gene)
VIF (viral infectivity factor gene)
VPU in HIV-I—May weaken transcriptional activator.
VPX in HIV-II—May be required for efficient budding.
- HIV is T lymphotropic, especially for monoclonal antibody and helper T cells. T4 (Leu-3).
- Cytopathic symptoms, including the development of multinucleated giant cells accompanied by cell death, are caused by virus infection.
- This describes the quantitative and functional depletion that is the signature of the lymphodepletion terminal case of Helps in the T4 lymphocyte subset.
- The T4 count (less than 60%), the non-specific proliferation of B lymphocytes that produce functionally incompetent wasted serum immunoglobulins (IG and IgA), and non-reactivity (energy) to remember antigens are decreased at the endpoint.
- The final result is complete lymph node loss, CMI deficiency, leaving the patient vulnerable to a wide variety of opportunistic infections (bacterial, viral, fungal, and parasitic).
Etiopathogenesis:
- T4 lymphocytes are affected by HIV by tainted sperm, polluted blood, and blood products, and occasionally by saliva, urine, and fecal matter.
- The outermost cover is lost at the entry site until the virus binds to the CD4 receptor.
- Subsequently, the inner protein coat is cast off and the naked enzyme RT transcribes DNA and viral RNA (norovirus).
- The viral DNA genome (provirus) interacts with the host DNA genome after its entry into the host nucleus.
- The T4 lymphocyte continues to live with provirus in the absence of immunological activation and the resulting introduction into host
- DNA is stalled, leading to latent infection with HIV.
- At this point, what affects viral replication or dormancy is unpredictable. Following its transcription, the viral messenger RNA (mRNA) redirects the host cytoplasmic machinery to synthesize the newer viral particles.
- Eventually, the cell dies and newly produced viruses develop out of the dying cell, leading to terminal lymphodepletion cases.
- The end-stage is marked by decreased T4 count (60%), the non-specific unrestrained proliferation of B lymphocytes that contain disproportionate incompetent usable wasteful immunoglobulins (IgG, IgA), and non-reactivity to retrieve antigens.
- A complete loss with the characteristic “burnt-out” image can be seen by the lymph node in the terminal point.
- The end result is a long-standing CMI disorder that leaves the infected individual exceptionally vulnerable to a wide variety of opportunistic diseases and malignancies of different forms that are life-threatening.
Clinical picture:
- It appears like the incubation cycle is long, spanning from 6 months to over 2 years. AIDS occurs in gays (75 percent), but there is also a chance of illness in gay men, heterosexuals, intravenous drug patients, and hemophiliacs infected with blood products or factor VIII.
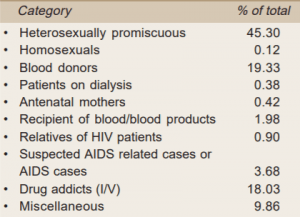
- AIDS is marked by pronounced immune system suppression, the production of irregular neoplasms, especially Kaposi’s sarcoma, or a broad range of serious opportunistic infections.
- Fatigue, malaise, unexplained lack of weight, fever, shortness of breath, persistent diarrhea, white tongue patches (hairy leukoplakia or oral candidiasis), and lymphadenopathy are some signs.
- Fungal (Pneumocystis carinii, Candida albicans, Cryptococcus neoformans, Histoplasma capsulatum, etc.), bacterial (Mycobacterium avium, Mycobacterium tuberculosis, Listeria monocytogenes, salmonella, Nocardia asteroides, etc and viral (Mycobacterium avium, Mycobacterium tuberculosis, Listeria monocytogenes, etc.) can be the most common complication of AIDS (cytomegalovirus, Herpes simplex, adenovirus, Hepatitis-B, etc.).
- HIV can invade other types of cells, such as in vivo B lymphocytes and monocytes, and a number of in vitro human cell lines.
- Viruses are present in the lymphoid cells, brain, thymus, spleen, and testes and can spread across the body.
- No animal models for AIDS have been created.
Inactivation of HIV:
10 minutes’ treatment at 37°C can inactivate this virus, with:
- 10% household bleach
- 50% ethanol
- 35% isopropanol
- 1% NP40
- 0.5% Lysol
- 0.5% paraformaldehyde
- 0.3% H2O2
Besides extreme pH (pH 1.0 and 13.0), heating at 56°C for 10 minutes can inactivate HIV.
Laboratory Diagnosis
Direct Methods
i. Cultivation of T lymphocytes: T lymphocytes of regular lymphocytes are cultured with interleukin on special cell lines (Hg, HUT78 U937). T cell stimulation and multinucleated giant cell demonstration can be performed within 2 to 20 weeks. It is the traditional way of verifying HIV infection.
ii. Detection of reverse transcriptase: It is possible on virus grown cells by radiolabeling.
iii. Solid-phase ELISA: It is useful to detect HIV antigen.
iv. Phase contrast microscopy: It is helpful in assaying the prevention of reclustering of MT-4 cells.
v. Electron microscopy: Demonstration of the fuzzy envelope of infected T4
vi. Animal study: Reproduction of human lesions in nonhuman primates has limited diagnostic importance.
Indirect Methods
Antibodies to HIV usually appear in 6 to 8 weeks after the exposure to the virus. The following methods are simple, easy, and quite useful to diagnose AIDS patients.
i. ELISA
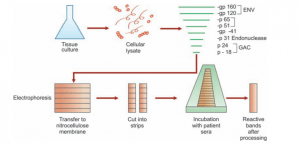
ii. Western Blot Assay:
- The HIV-specific antigen fractions initially resolved by the SDS polyacrylamide gel are moved by electroplating to the nitrocellulose membrane.
- The membrane antigenic profile includes, in increasing order of molecular scale, P17, P24, P31, gp41, P55, P56, gp160
- Reaction with HRP labeled anti-IgG antibody and chromogen substrate reaction are the latter steps.
- The formation of pink-colored bands shows the location on the membrane of the specific antigen-antibody complex.
- The IgM-Western Blot Assay test, however, varies slightly from the Western Blot Assay test.
- The basic procedure of this test is similar, with two exceptions being diaminobenzidine as a substrate and P24 as a positive control.
- In addition to the brown aspect resolution, the location of the immune complex is indicated.
- A classic HIV infection is associated with the appearance of all three gene products (env, gag, and pol).
- Otherwise, two bands of env (gp41, gp120) also display a positive sequence. ELISA often gives rise to false-positive results due to antibodies that cross-react with T4 lymphocytes, especially in multiparous women. This is never used in the Western Blot system.
iii. Radio-immunoprecipitation assay: This technique involves radioactive antigen.
iv. Polymerase chain reaction:
- Modern and exciting science is polymerase chain reaction (PCR). The identification and treatment of genetic, oncological, hematological, and infectious disorders are being widely used.
- In this procedure, disease-specific sequences of either RNA or DNA from the tissue or body fluid of the patient are specifically identified.
- It is very fragile.
- This approach is commonly used in the infection of HIV. It is helpful in tracking the success of antiviral chemotherapy, in addition to quantitative PCR techniques.
v.Dot blot hybridization.
vi. Agglutination tests using RBC/latexgelatin, colloidal gold, Immuno dot/strip, and PAT (particle agglutination tests).
vii. Detection of antibody to nef gene product (27 KD protein) along with p20 and gp120.
viii. Fujerbio agglutination test: In this test, antigen-coated gelatin particles are
agglutinated by antibodies present in the serum of the patient. It is quite a simple and convenient test. However, false-positive reactions do occur.
ix. Karpas test:
- HIV contaminated cells are fixed in this test on Teflon coated slide wells to which the patient’s serum is applied.
- Antihuman immunoglobulin called horseradish peroxidase is added after some time. A fitting and corresponding substrate is added later.
- If the test is positive, color evolves.
- When the test is negative, no color emerges.
- Slide immunoperoxidase monitoring is easy to perform and not costly.
Surrogative markers:
They are direct predictors of HIV infection and are:
1. Low CD 4 cells
2. Low B2 microglobulin
3. Increased neopterin
References
- http://tohealthmedico.blogspot.com/2016/04/hiv-positive-vs-aids.html
- https://faculty.psau.edu.sa/filedownload/doc-15-ppt-4af0e3f08d279f5e0fa660bc86b70c78-original.ppt
- https://kupdf.net/download/gupte-the-short-textbook-of-medical-microbiology-including-parasitology-10th-edition_5910e717dc0d60934e959ebf_pdf
