Contents:
Introduction
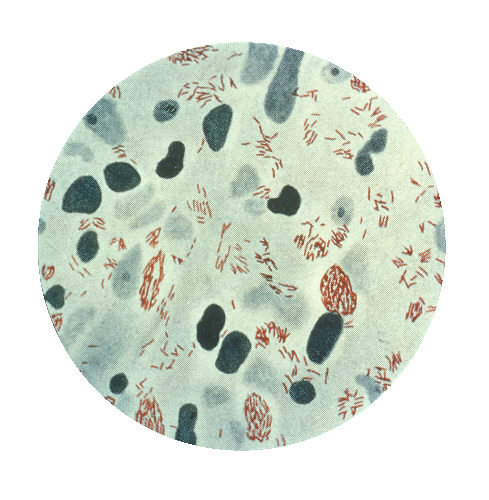
Mycobacterium leprae, the causative agent of leprosy (Hansen’s disease), presents one of the most intriguing life cycles in bacterial pathogenesis. This comprehensive guide explores the complex journey of this obligate intracellular pathogen, from transmission to multiplication within host cells.
What is Mycobacterium leprae?
Mycobacterium leprae is an acid-fast bacillus discovered by G.H. Armauer Hansen in 1873, making it the first bacterium identified as causing disease in humans. This slow-growing organism has several unique characteristics:
| Characteristic | Description |
|---|---|
| Size | 1-8 μm in length, 0.2-0.5 μm in width |
| Shape | Rod-shaped, slightly curved |
| Growth Rate | Generation time of 12-14 days |
| Temperature Preference | Optimal growth at 27-30°C |
| Special Features | Cannot be cultured on artificial media |
The Unique Characteristics
Mycobacterium leprae exhibits several distinctive features that make it particularly challenging to study:
- Obligate Intracellular Nature
- Cannot be grown in artificial culture media
- Requires living cells for survival and reproduction
- Shows preference for Schwann cells and macrophages
- Temperature Sensitivity
- Thrives in cooler areas of the human body
- Optimal temperature range explains disease patterns
- Affects peripheral nerves and skin predominantly
Life Cycle Stages
The life cycle of M. leprae can be divided into several key stages:
Stage 1: Entry into Host
- Primary route through respiratory droplets
- Secondary routes via broken skin
- Initial interaction with host immune cells
Stage 2: Cell Entry and Establishment
- Attachment to host cells (primarily Schwann cells)
- Phagocytosis by macrophages
- Evasion of host immune response
Stage 3: Multiplication
- Slow binary fission (12-14 days)
- Accumulation within host cells
- Formation of globi (clusters of bacteria)
Stage 4: Spread and Dissemination
- Movement to adjacent cells
- Transport via lymphatic system
- Establishment in new tissue sites
Host Interaction and Transmission
M. leprae’s interaction with host cells is complex and multifaceted:
- Initial Contact
- Recognition of surface molecules
- Attachment to specific receptors
- Triggering of cellular responses
- Cellular Entry
- Phagocytosis by host cells
- Modification of phagosomal environment
- Establishment of survival niche
- Transmission Dynamics
- Primary transmission through prolonged close contact
- Respiratory route predominant
- Environmental factors affecting transmission
Clinical Significance
Understanding the life cycle is crucial for:
- Disease Management
- Early detection strategies
- Treatment timing optimization
- Prevention of transmission
- Public Health Measures
- Contact tracing
- Infection control
- Community health programs
Prevention and Control
Effective control measures include:
- Early Detection
- Regular screening of contacts
- Community surveillance
- Healthcare worker training
- Treatment Strategies
- Multi-drug therapy (MDT)
- Contact prophylaxis
- Follow-up care
Frequently Asked Questions
Q: How long does it take for M. leprae to show symptoms after infection? A: The incubation period can range from 2 to 20 years, with an average of 5-7 years before symptoms appear.
Q: Can M. leprae survive outside the human body? A: The bacterium can survive outside the human body for up to 9 days in optimal conditions, but cannot multiply without a host.
Q: Is leprosy highly contagious? A: No, leprosy is not highly contagious. It requires prolonged close contact with untreated individuals for transmission.
Q: Can animals carry M. leprae? A: Yes, armadillos are known natural reservoirs of M. leprae and can transmit the disease to humans.
Q: Is there a vaccine for leprosy? A: While BCG vaccine offers some protection, there is no specific vaccine for leprosy. Research is ongoing.
Important Medical Disclaimer
This article is provided for educational and informational purposes only. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment.
If you suspect you have been exposed to Mycobacterium leprae or are experiencing any symptoms related to leprosy:
- Seek immediate medical attention
- Consult a qualified healthcare provider
- Do not delay getting professional medical help
- Do not attempt self-diagnosis or treatment based on this information
Early diagnosis and proper medical treatment are crucial for managing leprosy effectively and preventing complications. Always consult with qualified healthcare professionals for medical advice.
References
- World Health Organization. (2023). Global leprosy update, 2022. Weekly Epidemiological Record.
- Scollard, D. M., et al. (2006). The continuing challenges of leprosy. Clinical Microbiology Reviews.
- Britton, W. J., & Lockwood, D. N. (2004). Leprosy. The Lancet.
- Cole, S. T., et al. (2001). Massive gene decay in the leprosy bacillus. Nature.
- Rodrigues, L. C., & Lockwood, D. N. (2011). Leprosy now: epidemiology, progress, challenges, and research gaps. The Lancet Infectious Diseases.
