Contents:
Sterilization: Physical and Chemical methods
- Sterilization, disinfection, antisepsis, asepsis, and chemotherapy refer to antimicrobial measures, which cause direct damage to infectious agents.
- Sterilization is a complex of physical and chemical methods of complete inactivation of all vegetative and dormant forms (e.g., spores) of any kind of microbial agent.
- Prevention of body microbial contamination during various medical manipulations is the main goal of sterilization in medicine.
- The sterilization is applied to all kinds of medical devices and substances – medical instruments, drugs, dressing and stitch materials, linen, culture media, laboratory utensils, etc.
- In microbiological practice, different sterilization methods are employed for the maintenance of aseptic conditions in laboratory work, protection of culture media and cell cultures from extraneous microbial contamination, for prevention of microbial biodegradation of drugs or laboratory reagents.
- All sterilization techniques can be divided into physical and chemical methods.
Physical methods of sterilization
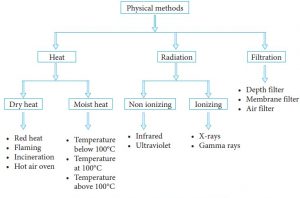
- It comprises a broad number of procedures based on various physical principles for sterilization
- Sterilization by heating, high pressure, mechanical sterilization (microbial filtration), sterilization by irradiation.
- One of the most reliable methods of sterilization is autoclaving. The sterilizing operation within autoclave is provided by contact of saturated overheated steam under elevated pressure with sterilized objects that result in the rise of temperature of sterilized things.
- Depending on sterilized materials, the temperature of saturated steam may be in the interval 110oC up to 138oC with additional pressure 0,4 up to 2,5 atmospheres and exposition time 30 to 60 minutes.
- Various nutrient media, isotonic sodium chloride solution, distilled water, the textile products are usually sterilized at 1 additional atmosphere at 121oC within 15-30 minutes.
- Monitoring of sterilization efficacy is performed by a number of mechanical, chemical, and biological indicators.
- Mechanical indicators of sterilization quality include the regular control of time, temperature, and pressure of sterilization cycles.
- Chemical indicators are used mainly in combination with biological ones. Chemicals are placed into packs with sterilized objects to confirm their exposure to sterilant (e.g., steam). These indicators are usually based on heat-sensitive inks that change color when sterilization parameter is achieved (temperature, steam-time, etc.)
- Biological indicators are most reliable for the control of various sterilization procedures. The viable microbial bodies with the highest resistance (spores of Geobacillus stearothermophilus or Bacillus atrophaeus) directly monitor the lethal effect of sterilization.
Heating with air
- In hot air ovens at 180oC and exposure time for 60 min is a highly effective sterilizing measure, but it may cause the decay of labile substances.
- The objects, poorly permeable for vapor, but resistant to heat (glass, ointments, hydrophobic materials) might be sterilized by this method.
- In dental practice, fast decontamination of all-metal dental or other instruments is performed with glass-perlen sterilizers operating at 190-290oC.
- Rapid inactivation of most of the microbial germs is achieved by immersion of medical instruments or their working parts into a chamber filled with overheated (250oC or more) minute glass beads for 0.5-3 min.
Flaming is a common method for sterilization in microbiology, primarily, for sterilization of wire loops, or outlets of the test tubes.
Incineration is used for the destruction of biohazardous wastes.
Tyndallization
- The fractional sterilization (or tyndallization) at 56-70°С for 1 hour within 5 days is used for media or medical substances with heat-labile contents (proteins, vitamins, etc.)
- During the intervals between sterilization events, the objects are placed into the thermostat at 37°С for overnight incubation.
- In this case, the spores, still remaining in sterilized medium, overgrow, and newly germinated vegetative cells will be destroyed at the next sterilization step.
Pasteurization
- It is not regarded as a method of complete sterilization.
- It is employed for partial rapid decontamination of milk, juices, wine, beer, and other products.
- It uses high-temperature, short-time treatment (at 72°С for 15 sec, or at 63°С for 30 min) with next cooling to 40°C.
- In combination with aseptic packaging the pasteurized milk can be stored in refrigerators for 2-3 weeks.
Sterilization of heat-labile substances
- The sterilization of heat-labile substances (vitamins, antibodies, and immune sera, biological products, or culture media) is achieved by filtration through bacterial filters with controlled standard porosity.
- Usually, the synthetic filters with 0.1-0.45 μm of pore sizes (cellulose acetate, nylon, polytetrafluoroethylene (PTFE), or others) are applied for filtration.
- These filters efficiently trap the bacteria and a large number of viruses, albeit the viruses of small sizes, as well as bacterial toxins, can pass through these filters without significant retention.
Sterilization by irradiation
- It uses radiation of various wavelengths. Ultraviolet germicidal irradiation (UV-irradiation) is performed with the short-wavelength UV-light (about 260 nm) that damages microbial DNA.
- It is broadly employed for air sterilization of wards and rooms in medical health care units.
- Heat-resistant instruments can be sterilized by infrared radiation (wavelength of 700-1000 nm) that inactivates microorganisms by heat generation.
- In industrial conditions ionizing gamma irradiation is used for sterilization of packed dressings, plastic disposable syringes, systems for blood transfusions, plastic Petri dishes, vitamins, hormones antibiotics, etc. Radioactive isotopes Co60 or Cs137 are introduced as the sources of gamma radiation that irreversibly damages the DNA of microorganisms.
For chemical sterilization
The various chemical substances are available – ethylene oxide gas, ozone, formaldehyde, glutaraldehyde, hydrogen peroxide, peracetic acid, ethanol, and some others.
- Ethylene oxide treatment is one of the most efficient methods of chemical sterilization. It inactivates all viable forms of microorganisms including bacterial spores, viruses, fungi. Ethylene oxide easily diffuses through the package covers, thereby about 50% of manufactured medical disposable devices are sterilized by this method.
- Ozone as sterilant gas is applied for sterilization and decontamination of air and water, for instance, for treatment of water in swimming pools.
- Peracetic acid and glutaraldehyde can be applied for sterilization of fiber optics, e.g. endoscopes.
For the control of the efficacy of sterilization various meter devices are used (thermometers, manometers) as well as thermochemical indicators with known melting points of controlling substances (urea, benzoic acid, and others). For biological control of sterilization, the strips with spores of heat-resistant bacteria Geobacillus stearothermophilus are placed into containers with sterilizing objects. These spores can withstand short-term exposure to a temperature of 121° C.
References
-
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC440886/
-
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3134674/