Contents:
Tumor Immunity
INTRODUCTION
Cancer is an abnormal, uncontrolled cellular growth. Risk factors linked to cancer include diet and obesity, family history of cancer, sedentary lifestyle, occupational factors, viruses and biological agents, alcohol, environmental pollution, and UV rays.
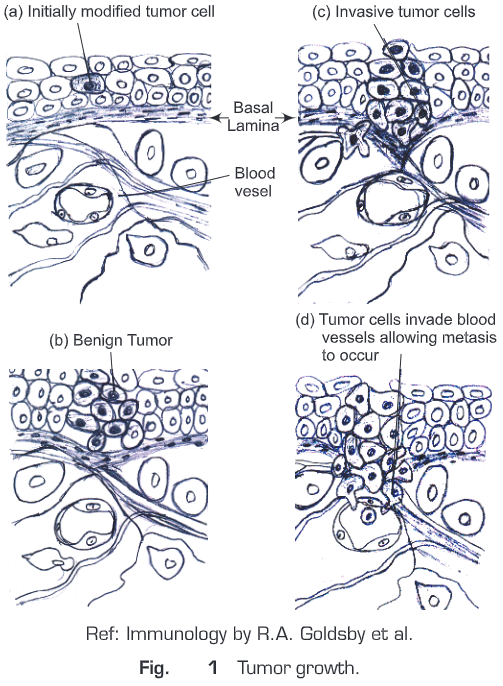
A tumor is an abnormal growth of body tissue and it may be benign and malignant (Fig.1)
- Benign tumor: not capable of indefinite growth and the host survives.
- Malignant tumor: Continues to grow indefinitely and spreads (metastasizes), eventually killing the host. This uncontrolled growth may be due to up-regulation of oncogenes and/or downregulation of tumor suppressor genes (which inhibit tumor growth often by inducing cell death).
Metastases are spread of cancer cells from one part of the body to another, invades the blood or lymphatic vessel and are carried to other tissues where they continue to proliferate. In this way a primary tumor at one site can give rise to a secondary tumor at another site.
Malignant tumors are classified on the basis of embryonic origin of the tissue from which it is derived. There are three types of malignant tissues:
- Carcinomas: Tumors that arise from endodermal/ ectodermal tissue such as skin or epithelial lining of internal organs. e.g. cancers of colon, breast, prostate and lung.
- Leukemias/Lymphomas: These are the tumors of hematopoitic cells of bone marrow.
Leukemias proliferate as single cell and lymphomas tend to grow as tumor mass.
- Sarcomas: Tumors that arise from mesodermal connective tissue such as bone, fat or cartilage.
MALIGNANT TRANSFORMATION OF CELLS
- Malignant transformation is the process by which cells acquire the properties of cancer and used extensively as model of cancer induction.
- This may occur as a primary process in normal tissue, or secondary in case of malignant degeneration of a previously existing benign tumor.
- In this process, normal cultured cells are treated with chemical carcinogens, radiations and certain viruses which can change the morphology and growth properties.
- Malignant transformation makes the cell able to produce tumor when they are injected into animals. Both cancer cells and transformed cells can be sub-cultured indefinitely for all practical purposes.
- Various chemical and physical agents are used to induce malignant transformation. Chemical agents: DNA alkylating reagent, polycyclic hydrocarbons and aromatic amines; Physical agents: UV light and ionizing radiations. This process involves two distinct phases: initiation and promotion.
Initiation: Changes in the genome but not exactly the malignant transformation.
Promotion: After initiation, malignant transformation occurs by stimulation of cell division by some promoters.
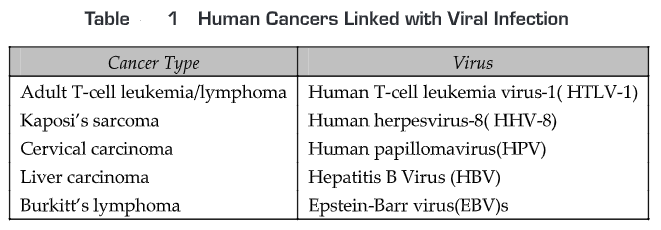
Polyoma and SV40 viruses have been linked to cancer in both experimental animals and humans. The DNA of both the viruses is integrated randomly into the host genome, including a number of genes that are expressed early in course of viral replication. SV40 encodes for two proteins: large T and little T and polyoma encodes three proteins: large T, middle T and little T. Each of these proteins plays an important role in malignant transformation. Human cancer-related viruses are EBV, HBV, HPV, SV40 and polyoma (Table.1). RNA viruses HTLV-1 and HHV-8 replicate in the cytosol and do not induce malignant transformation except retrovirus (e.g. Rous sarcoma virus).
TUMOR-ASSOCIATED ANTIGENS
To react against a tumor, the immune system requires some antigen. A number of alterations in gene expression occur in cells during tumorigenesis. Tumorigenesis may give rise to expression of new antigens called neo-antigens or alteration in existing antigens that are found on normal cells. These antigens may include membrane receptors, regulators of cell cycle and apoptosis or molecules involved in signal transduction pathways.
There are two main types of tumor antigens:
- Tumor-specific transplantation antigens (TSTA) which are unique to tumor cells and not expressed on normal cells. They are responsible for rejection of the tumor (Fig. 2)
- Tumor associated transplantation antigens (TATA) that are expressed by both tumor cells and normal cells (Fig. 2).
Although chemical, UV- or virus-induced tumors express neo-antigens, the majority of these tumors are often weakly immunogenic/ non-immunogenic. TSTAs cannot be identified easily in most cases. Some of these antigens may be secreted while others may be membrane-associated molecules:
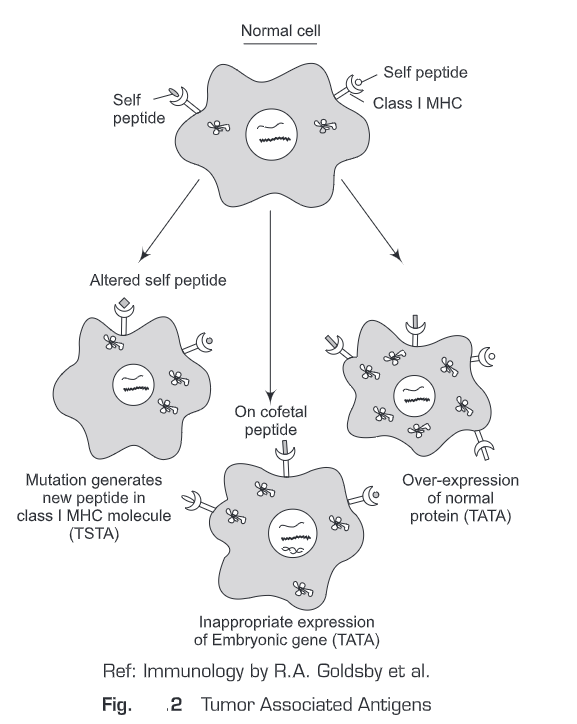
Tumor associated transplantation antigens (TATA): The majority of tumor antigens is also present on normal cells and is referred to as tumor associated transplantation antigens. They may be expressed at higher levels on tumor cells when compared to normal cells. Alternatively, they may be expressed only during development of cells and lost during adult life but re-expressed in tumors.
Tumor-associated developmental antigens/ oncofetal antigens: These include alpha-fetoprotein (AFP) and carcinoembryonic antigen (CEA) found secreted in the serum. AFP is found in patients with hepatocellular carcinoma whereas CEA is found in colon cancer. These are important in diagnosis. AFP is produced as a secreted protein and CEA is found both on cell membranes and in secreted fluids. Since secreted antigens contribute little toward immunity against tumors, the role of these neo-antigens in immuno-surveillance is not clear. The normal range of AFP concentrations in humans is 0-20 ng/ml. This level rises in patients suffering from hepatomas and non-seminal testicular carcinoma. AFP level may also be raised in some non-malignant conditions, such as cirrhosis, hepatitis and other forms of liver da CEA levels in normal people range up to 2.5 ng/ml, but they increase significantly in certain malignancies, particularly colorectal cancers.
They may also rise in some non-malignant conditions.
Tumor associated transplanted antigens on viral tumor—Viruses that cause human tumors include:
- DNA viruses
- Papova (papilloma, polyoma) viruses: Papilloma virus causes cervical cancer.
- Hepatitis virus: Hepatitis B virus causes hepatocellular cancer.
- Adenoviruses may also be tumorigenic
- RNA viruses
- Retroviruses: Human T-lymphotropic viruses (HTLV-I and HTLV-II) causes T cell leukemias.
A number of viruses cause different types of tumors in animals (for example, SV-40 virus, adenovirus, Rous sarcoma virus, Friend erythroleukemic virus, Moloney Rauscher and Gross viruses). Viruses are involved or suspected to be involved in some human malignancies (HTLV-1 in leukemia, hepatitis-B virus in hepatic carcinoma, papilloma virus in cervical cancer). Virus-induced tumors express cell surface antigens (distinct from antigens of the virion itself) which are shared by all tumors induced by the same virus. These antigens are characteristic of the tumor-inducing virus, regardless of tissue origin of the tumor or animal species in which the tumor exists.
Tumor associated transplantation antigens on chemically induced tumors—Chemically-induced tumors are different from virally-induced tumors in that they are extremely heterogeneous in their antigenic characteristics. Thus, any two tumors induced by the same chemical, even in the same animal, rarely share common tumor specific antigens. These unique antigens on chemically- induced tumors are referred to as tumor specific transplantation antigens (TSTA),.
TUMOR EVASION OF THE IMMUNE SYSTEM
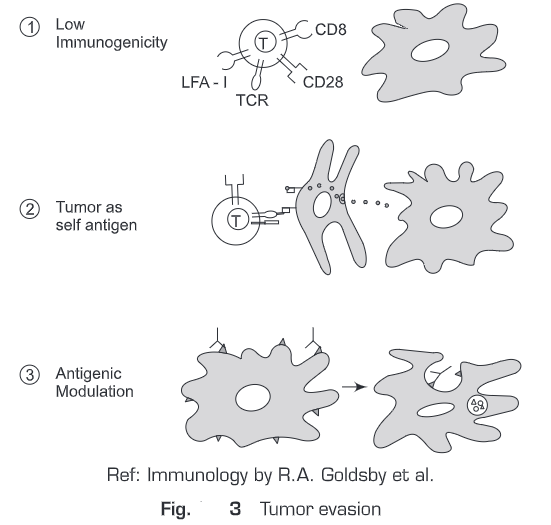
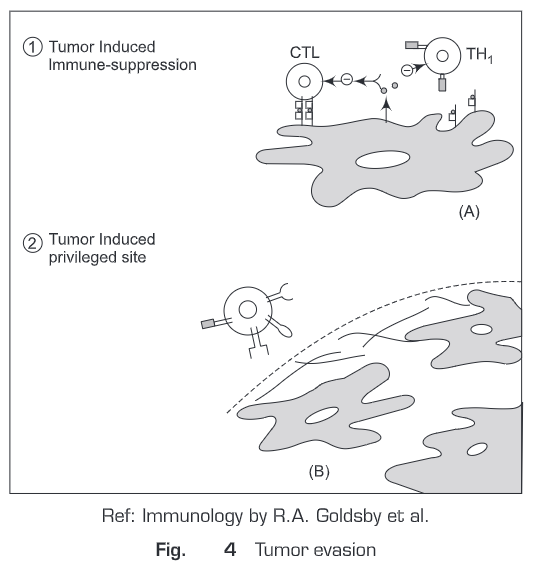
Many individual die each year from the cancer suggest that immune response to tumor cell is not effective. There are five mechanisms by which tumor cells appear to evade the immune system.
- Tumor treated as self antigen: Tumor antigens are taken up and presented by APCs in absence of co-stimulation tolerize T-cells (Fig. 3).
- Low immunogenicity: T-cells activation requires co-stimulatory signal which is triggered by peptide-MHC complex. In absence of peptide -MHC molecule complex, no co-stimulatory signals are produced (Fig. 3).
- Antigenic modulation: Antibody against tumor cell surface antigens can induce endocytosis and degradation of the antigen. Immune selection of antigen loss variants occur (Fig. 3).
- Tumor induced Immune suppression: Factor TGF-B secreted by tumor cells inhibits T-cells directly (Fig. 4).
- Tumor-induced privileged site: Factor secreted by tumor cell creates a physical barrier to the immune system (Fig. 4).
ONCOGENES AND CANCER INDUCTION
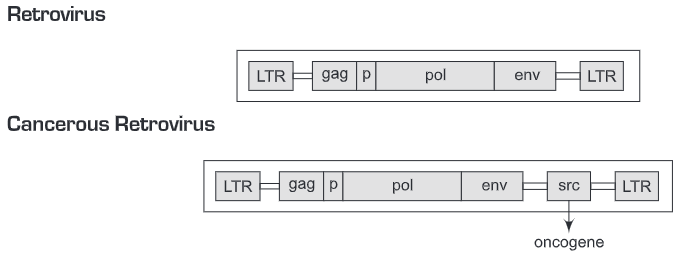
Retroviruses are RNA viruses that cause cancer in variety of animals and humans. This virus is made of three main genes gag, pol and env that are required for virus replication and do not play role in cell transformation. A retrovirus can transform cells from normal to cancer if they include a specific gene that is capable of inducing cell transformation and this gene is known as oncogene.
Types of oncogenes:
- Viral oncogene: gene from the retrovirus itself
- Non-Viral oncogene/Cellular oncogene: The genes of the host cell that are in an inactive form usually and if the gene incorporates with the viral genome then it will form a highly oncogenic virus.
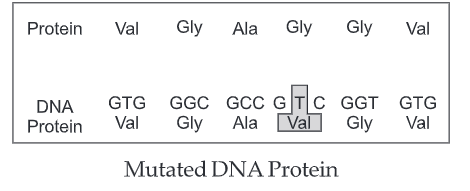
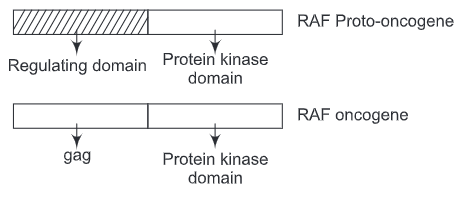
Proto-oncogenes: Proto-oncogenes are the form of cellular genes that inactive normally but can incorporate with the viral genome to produce a highly oncogenic virus. The proto-oncogene can be converted to an oncogene in four ways:
- Mutation
- Abnormal activity
- Gene Translocation
- Amplification
- Mutation:
Mutation in Ras gene
↓
Continuous activation of Ras (constitutively in the GTP-bound conformation)
↓
Unregulated a proliferation
↓
Cell transformation
- Abnormal Activity:
Removal of the Regulatory domain in the Raf gene and replaced by gag gene
↓
Raf kinase domain consciously active
↓
Cell transformation
- Gene translocation:
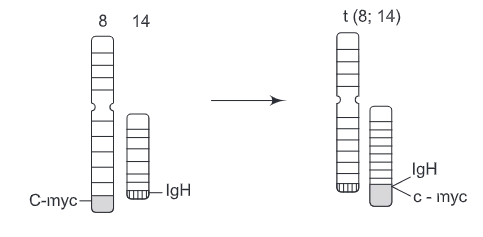
c-myc gene is translocated from chromosome 8 to the IgH on the chromosome 14 resulting in abnormal c-myc expression
↓
Cell transformation
- Amplification:
(a) Amplification of n-myc
↓
neuroblastoma.
(b) Amplification of erbB-2
↓
Breast and ovarian carcinomas
Functions of oncogene
- Growth Factor: Epithelium growth factor ( EGF) and platelet-derived growth factor (PDGF)
- Growth Factor Receptor: Receptor for colony-stimulating factor (fms), Receptor for epidermal growth factor (erb B)
- Signal transudation: GTP-binding protein with GTPase activity (Ha-Ras, N-Raf )and Tyrosine kinase (src)
- Transcription Factor: Component of transcription factor (Jun, Fos) and DNA binding protein (myc)
Questions
1. What is cancer? What are the risk factors linked to cancer?
2. Differentiate between benign and malignant tumor.
3. Discuss the classification of malignant tumor.
4. Explain the malignant transformation of cells.
5. Give some examples of human cancers linked with viral infections.
6. What do you mean by tumor antigens? Discuss.
7. Differentiate between TATA and TSTA.
8. What are oncogenes? Give examples.
9. Discuss the tumor evasion of the immune system.
10. How are proto-oncogenes converted to oncogenes?
11. What are the functions of oncogenes?