Introduction
The cell requires materials for growth, repair of worn-out structures and source of energy for these activities. The food material we eat serves these purposes. Thus, a regular supply of food is the need of the body. The food we eat contains complex substances and it is necessary to convert these complex substances into simpler forms; so that they can be absorbed into blood and transported to the cells for utilization. This conversion of complex food into a simple form, making it suitable for absorption is described as digestion of food.
This conversion is both mechanical and chemical. The organs that cause mechanical splitting of food include teeth, tongue and muscles that help in mastication and peristaltic movement in the gastrointestinal tract. The chemical conversion is caused by the secretory action of alimentary canal and the secretions produced and poured into it by the glands, i.e. salivary glands, liver and pancreas.
Thus, the organs involved in and constituting the digestive system are placed into two groups:
1. The alimentary canal; a long tube starting from mouth extending up to the anus and
2. Accessory organs, i.e. teeth, tongue, salivary glands, liver and pancreas.
The Alimentary Canal
It is 09 metres long tube extending from the mouth to the anus; through which the food passes. It serves the following functions:
- Receiving the food (Ingestion).
- Onward transmission of food (Peristalsis).
- Mechanical splitting of food.
- Chemical splitting of food.
- Absorption of food and
- Elimination of unabsorbed food residue (Excretion).
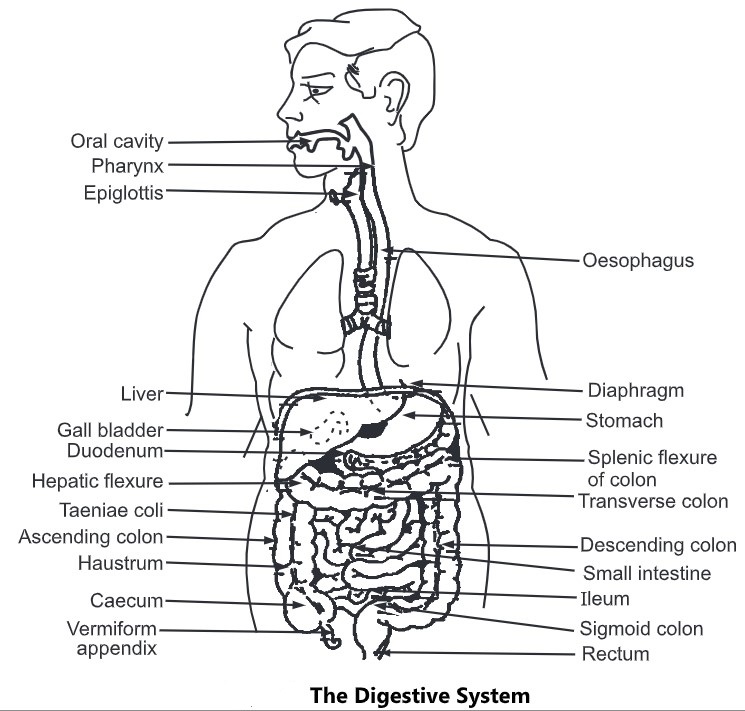
On the basis of structural peculiarities, the alimentary canal comprises:
- Mouth cavity
- Pharynx
- Oesophagus
- Stomach
- Small intestine
- Large intestine
- Rectum and anus
(1) Mouth Cavity
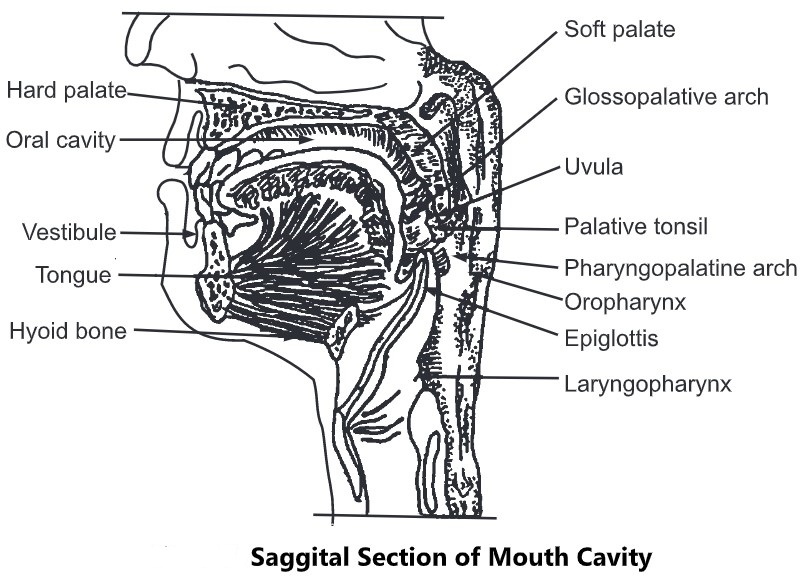
- The alimentary canal begins at the mouth. The mouth or oral cavity extends from the lips to the oropharynx.
- The roof of the mouth cavity is formed by a hard anterior bone palate; it is soft on the posterior. From the posterior margin of the soft palate, a small muscular flap hangs down called as uvula.
- The soft palate is attached to the tongue by the gloss palatine arches and to the wall of the oropharynx by the pterygopalatine arches.
- The palatine tonsils are composed of lymphoid tissue and are located in the fosse between the two arches. The floor of the mouth cavity is occupied by the tongue.
- The mouth cavity consists of two parts, the outer vestibule and the inner mouth cavity proper. The vestibule is the space outside the gum and teeth and inside the lips and cheeks.
- The lips, cheeks and tongue help in moving the food between upper and lower teeth during mastication (chewing).
Teeth and Mastication
- Teeth develop within sockets of the alveolar processes of maxillae and mandible. Dense connective tissue covered by smooth mucous membrane, the gums, covers these processes and extends a little way into each socket.
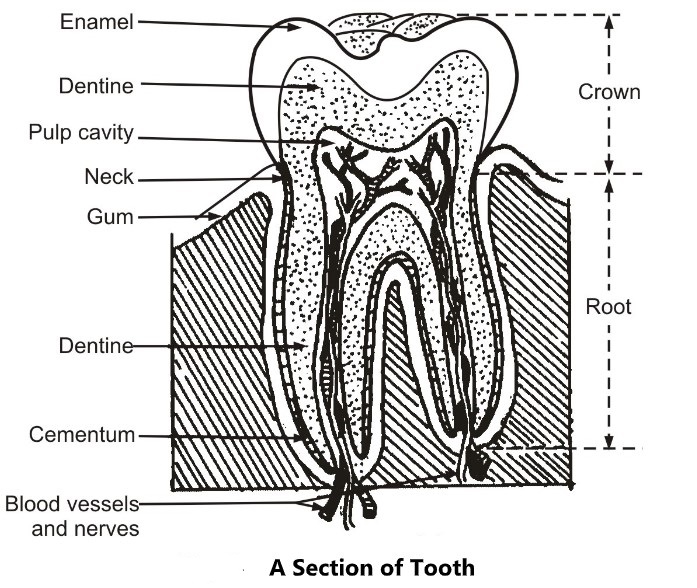
- The sockets are lined with a fibrous membrane called the periodontal membrane. A tooth possesses a crown, neck and root. The crown projects above the gum, the neck is surrounded by the gum and the root is beneath it.
- A tooth is made up of a very hard material called dentin. The dentin of the crown is covered by enamel, which is harder than dentin. A bone-like substance called cementum covers the dentin of the root and anchors the tooth to the periodontal membrane that lines the sockets.
- The central part of the tooth contains the pulp cavity that shows a connective tissue called the pulp, the blood vessels and nerves.
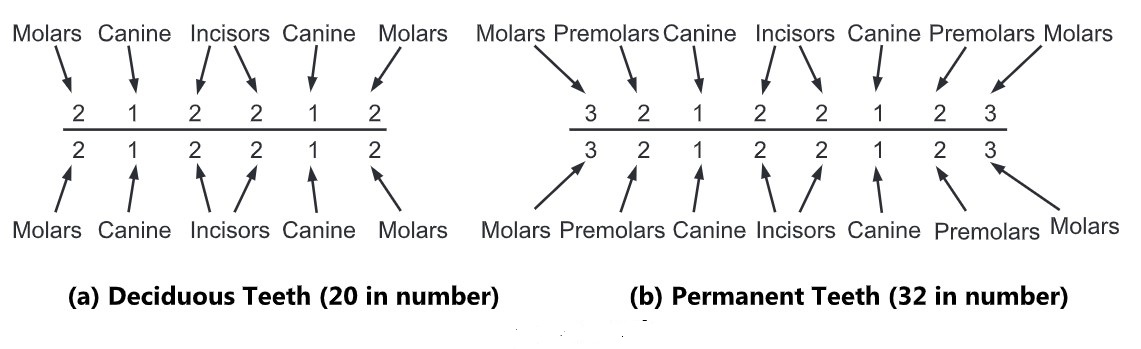
- There are four types of teeth; named on the basis of their shape. The incisors are chisel-shaped, the canines are cone-shaped and the premolars and molars have broad crowns with rounded cusps.
- In the lifetime of each individual normally two types of teeth are developed deciduous teeth or milk teeth, and permanent teeth.
- Mastication is the main function of the teeth. It involves biting and grinding food between the upper and lower teeth. Movements of the tongue and cheeks and lips assist in moving the food against the hard palate and the teeth.
The Salivary Glands
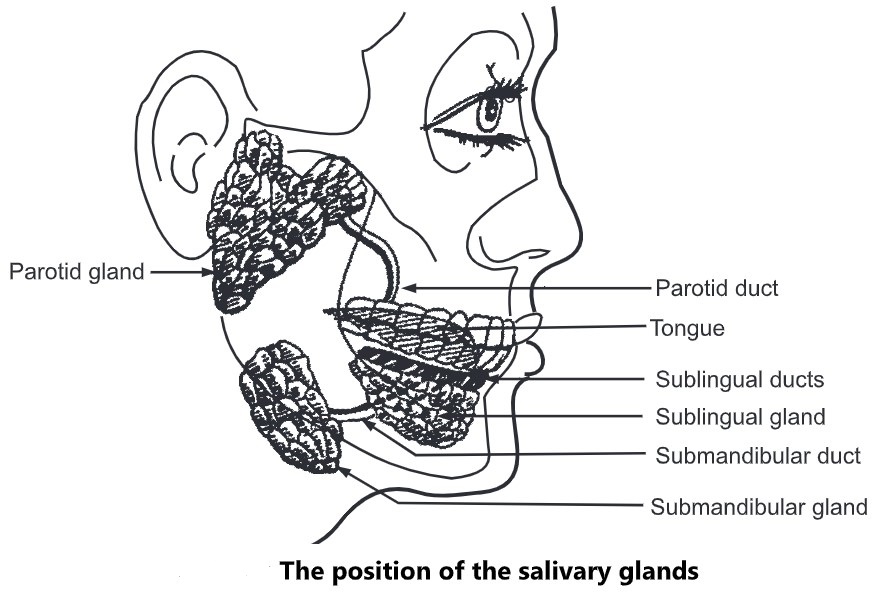
- The three pairs of salivary glands are the parotid, submandibular and sublingual glands. The parotid glands are the largest.
- They lay one on each side below and slightly in front of the ear. The submandibular glands are present on each side, beneath the Jaw-bone and the smallest sublingual glands lie beneath the tongue on each side.
- The function of the salivary glands is the secretion of saliva which is stimulated by the sight, smell and the presence of the food in the mouth. Saliva moistens the mouth, cleanses the tongue and makes speech easier.
- The enzyme ptyalin acts on cooked starches in an alkaline medium and converts them to a soluble form called maltose. The action of the enzyme continues till the food is rendered acidic by the action of gastric fluid.
- The saliva is the secretion from salivary glands and the mucous is secreted by glands of the mucous membrane of the mouth cavity; poured into it.
- It consists of water, mineral salts, salivary amylase (ptyalin) and mucous. Parasympathetic nerves supplied to salivary glands stimulate the secretion of saliva while sympathetic nerves depress the secretions.
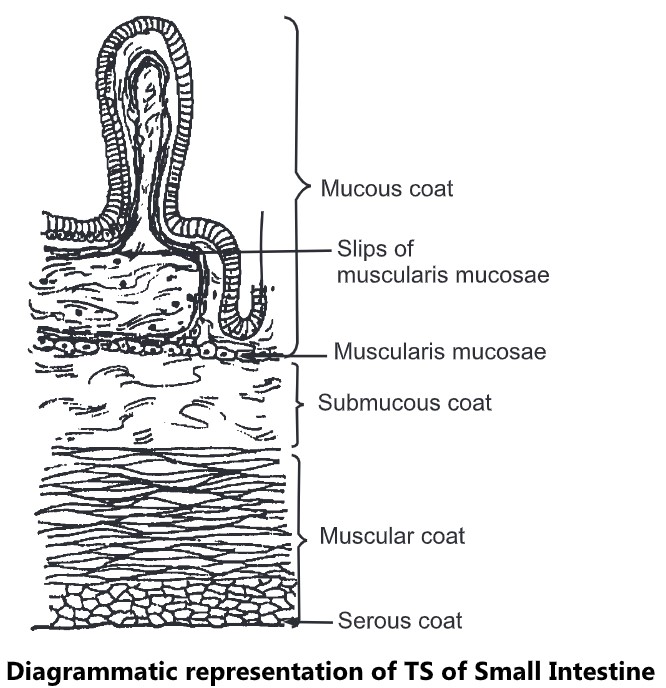
- The structure of the alimentary canal follows a consistent pattern from the oesophagus onwards. The walls of the alimentary canal are made up of the following four layers of tissues.
- Adventitia, the outer covering consisting of the Peritoneum in the abdomen.
- The muscle layer consists of both longitudinal and circular muscles.
- The submucous layer of loose connective tissue.
- Mucous membrane lining consists of epithelial cells.
In different regions of the digestive tract, there are certain modifications in these basic layers. The general structure of these layers is as follows:
(a) Adventitia
The outermost layer of the digestive tract is primarily composed of connective tissue. In the thorax region (i.e. in the case of the oesophagus) this connective tissue merges into the connective tissue of surrounding structures. In the abdomen, this covering forms the peritoneum. The peritoneum consists of two layers the parietal and the visceral. In this case, the outer layer is called the serosal.
(b) Muscle Layer
It consists of double layers of muscles, the inner layer in which the muscles are arranged circularly around the tube while in the outer layer the muscles are arranged longitudinally along the long axis of the tube. At different points along the tract, the fibres of the circular layer are thickened to form sphincters that guard the movement of food from one region of the tract to the other. The rhythmic contractions of these muscles produce peristalsis that propels the food onwards.
(c) Submucous Layer
It is composed of a thick layer of areolar connective tissue and contains blood vessels, lymphatic, and nerves.
(d) Mucous Membrane
This innermost lining of the tract has three distinct layers:
(i) The epithelial layer that borders on the lumen. It is a simple columnar epithelium throughout the tract except in the oesophagus where it is a stratified squamous epithelium.
(ii) The areolar connective tissue to which the epithelial cells are attached and
(iii) Outside of areolar tissue, a thin layer of smooth muscle fibres called the muscularis mucosa.
(2) Pharynx
- A muscular cone shaped tube, situated behind the nasal cavity, oral cavity and larynx. The base of the cone is above while the apex is below.
- It communicates with nasal cavity, mouth cavity and larynx on the anterior side. The part of pharynx behind nasal cavity and into which the nasal cavity opens is known as the nasopharynx.
- Like the nasal cavity, the nasopharynx is linked with pseudostratified columnar epithelium. On the lateral sides the auditory tubes open into the nasopharynx.
- The part of pharynx located behind mouth cavity and into which it opens is known as oropharynx. The mucous membrane of oropharynx is composed of stratified squamous epithelium.
- The laryngopharynx extends from oropharynx above to the larynx and oesophagus below. It is lined with stratified squamous epithelium and like oropharynx it serves as a passageway for both food and air. The laryngopharynx continues downwards as oesophagus.
(3) Oesophagus
It is a muscular tube that continues from pharynx above and opens into the stomach below. It is situated behind trachea and passes through mediastinum of the thorax. It pierces the diaphragm and enters into the abdomen, where it opens into the stomach. The peristaltic movement of the oesophagus moves the food towards the stomach.
(4) Stomach
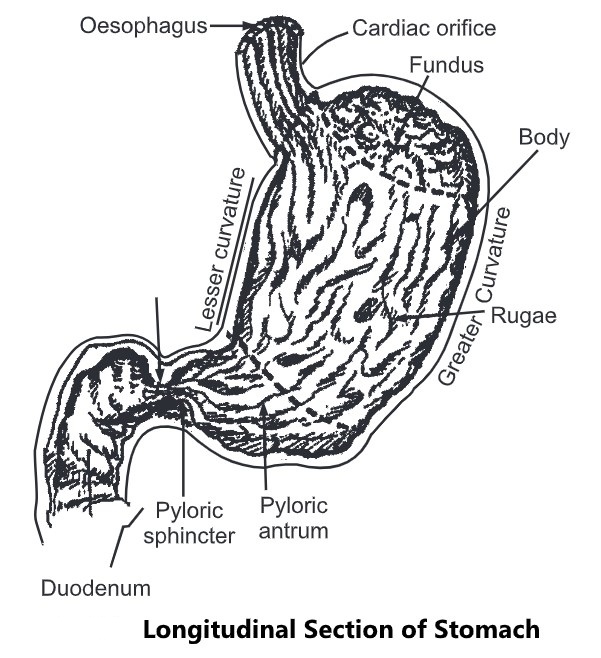
- It is the most dilated part of the alimentary canal lying just below the diaphragm; obliquely in the epigastric, umbilical and left hypochondriac regions of the abdominal cavity.
- It is a collapsible bag-like structure serving as a temporary reservoir for food. The oesophagus opens into the stomach at the cardiac orifice and duodenum continues from it at the pyloric orifice.
- It is ‘J’ shaped and shows two curvatures termed as the greater curvature and lesser curvature.
- The part of the stomach above the cardiac orifice is called the fundus, the main middle part is the body and lower part is the pyloric antrum.
Organs associated with the stomach.
Anteriorly – Anterior abdominal wall and left lobe of liver.
Posterior – Pancreas, spleen, abdominal aorta and left kidney
Superiorly – Diaphragm, oesophagus, left lobe of liver
Inferiorly – Transverse colon and small intestine
To the right – Right liver lobe and duodenum
To the left – Spleen and diaphragm
- Four layers of tissues as described in the general structural pattern of the alimentary canal are found in the stomach.
- Of these layers, the muscle layer is modified to show three layers of smooth muscle fibres: the outer layer of longitudinal fibres; the middle layer of circular fibres; and the inner layer of oblique fibres.
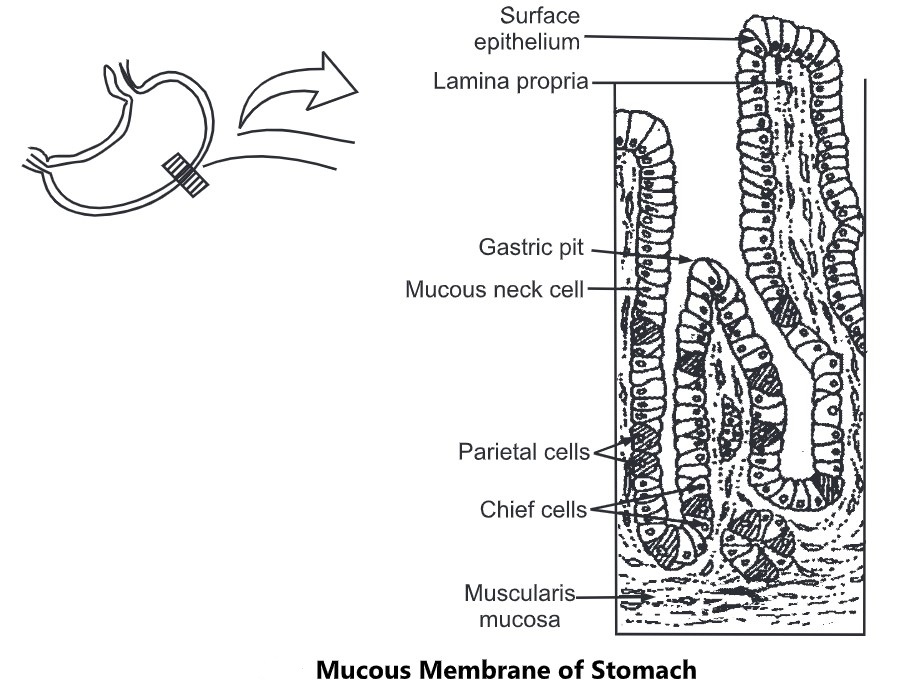
- This characteristic arrangement allows for strong muscular action causing churning motion and peristaltic movements. The mucous membrane lining is made up of columnar epithelial cells.
- When the stomach is empty, the mucosa and submucosa layers form longitudinal folds called as rugae.
- There is a large number of gastric glands situated below the surface of the mucous membrane.
- There are three kinds of such glands; those situated in the fundus and bodies of the stomach are the fundic glands, those in the cardiac region are the cardiac glands and in the pyloric region are the pyloric glands.
- The fundic glands contain different types of cells, of which the chief cells secrete pepsinogen and the parietal cells secrete hydrochloric acid. The cardiac and pyloric glands secrete mucous.
Gastric Juice and Functions of the Stomach:
- When the meal has been taken, the food accumulates in the stomach in layers. The muscle contractions cause churning movement that breaks down the bolus and mix it with gastric juice.
- When the muscles of the stomach are active the pyloric sphincter remains closed. After the contents are sufficiently liquefied, (Liquefied acidic food content of the stomach is called as chime) the strong peristaltic contractions of pyloric antrum forces gastric contents through the pylorus into the duodenum in small spurts.
The gastric juice is the secretion of gastric glands and is composed of
| Water Mineral salts Mucus Hydrochloric acid Intrinsic factor Pepsinogens Gastric lipase | About 2 — 3 litres of gastric juice is produced per day. The pH of gastric juice is 2 – 4. |
There are three phases of gastric secretions as follows:
(a) Cephalic phase
The secretion of juice in response to site, smell and thought of food is known as cephalic phase. It is the result of reflex stimulation of the vagus nerves.
(b) Gastric phase
The entry of food in the stomach stimulates the production of the hormone gastrin which enters in blood. This hormone, on reaching through blood to the gastric glands enhances, the secretion of gastric juice. This phase is known as gastric phase.
Sometimes Gram-negative bacillus H. pylori colonizes antral mucosa causing local inflammation and elevated gastrin and hydrochloric acid secretion. Presence of the organism is linked to peptic ulcer.
(c) Intestinal phase
- In this phase, the secretion of juice reduces in response to the hormone complex enterogastrone that is released from the small intestine as soon as food from the stomach enters the intestine.
- The water from the gastric juice assists in further liquefying food in the stomach. The acid medium generated by hydrochloric acid favours digestive processes in the stomach.
- The pepsinogen is activated to pepsin in this medium. It acts on proteins. Hydrochloric acid kills many micro-organisms that may prove harmful to the body.
- The intrinsic factor is useful for the absorption of Vitamin B12. The mucous lubricates the food and forms a protective barrier on gastric mucosa, protecting it from the contents of gastric juice.
- The stomach acts as a temporary reservoir of food. The muscular actions of the stomach mix the food with digestive juice and propel it further to the small intestine. The gastric juice with its enzyme begins the digestion of proteins.
- The gastric lipase acts on fats converting them into fatty acids and glycerol. Certain substances (e.g. water, alcohol, and some drugs) are absorbed from the stomach in the venous circulation.
(5) Small Intestine
- It is a long tube extending from pyloric sphincter of stomach up to ileocaecal valve. It is the most convoluted portion of the digestive tract.
- It is about 05 metres in length and lies in the abdominal cavity, surrounded by the large intestine. It has three regions which are continuous with each other. The three regions are duodenum (25 cm) followed by jejunum (02 metres) and ileum (03 metres).
- The duodenum is curved around the head of pancreas and is tightly attached to posterior abdominal wall.
- The common bile ducts from liver and pancreatic duct from pancreas join together and open into the duodenum at about its midpoint.
- The opening of these ducts is guarded by the sphincter of oddi. The jejunum is the middle region and is suspended in the abdominal cavity by the mesentery.
- The ileum is the terminal 03 metres long region and opens into the caecum of large intestine.
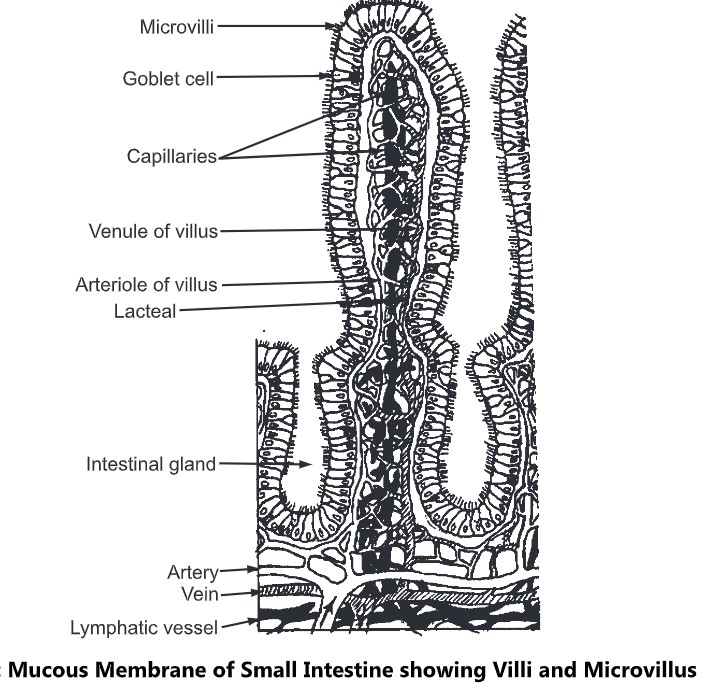
- Four layers of tissues as described in the general structural pattern of alimentary canal are found in the small intestine. However, the modification in the wall of the small intestine is in the submucosa and mucous layers.
- These layers extend into the lumen forming shelf-like folds, increasing the surface area of mucous membrane lining. The surface area is further increased by the presence of the large number of finger like projections of mucous membrane. These projections are known as villi.
- Within each villus is a lymphatic capillary called a lacteal that is surrounded by a network of blood capillaries.
- The columnar epithelial cells that form the mucous membrane of small intestine, at their free surface shows many folds, forming smaller projections called as microvill.
- The mucous membrane also shows presence of mucous secreting goblet cells. Between the villi are found the intestinal glands (crypts of lieberkuhn) that empty their secretions between the villi.
Intestinal Secretions and Functions of Small Intestine
- The Bruner’s glands located in duodenum and the goblet cells of intestinal mucosa secrete mucous.
- The secretion of mucous by Bruner’s glands is stimulated by intestinal hormone secretin, the vagal impulses and the irritating stimulation of the mucosa.
- The entry of liquefied acidic food (chime) from stomach into the intestine stimulates goblet cells to secrete mucous.
- The distension or irritation of intestinal mucosa and to some extent vagal impulses stimulate intestinal gland to secrete the intestinal juice called the succus entericus.
- The composition of intestinal juice is as follows:
| Water Mineral salts Enterokinase Amylase Peptidase Lipase Sucrase Maltase Lactase | About 2 — 3 litres of intestinal juice is produced per day. The pH of this juice is 7 – 9. |
- Much of the food that enters the small intestine is undigested, though digestion of proteins and starches have commenced in prior parts of the alimentary canal.
- Major digestion and absorption of food occurs in small intestine. The movements of intestine and chemical action of digestive juices contribute to digestion process in the small intestine.
- The muscular movements of small intestine apart from mixing food with digestive juices assist in absorption as absorbable materials are brought in contact with mucosa and improve the blood supply to the intestine which helps in secretion and faster removal of absorbed food. These movements include peristaltic, rhythmical and pendulum movements.
- The peristalsis is defined as a wave of relaxation (caused by contraction of longitudinal muscles) followed by a wave of constriction (caused by constriction of circular muscles). This helps in propelling the food contents onwards.
- The rhythmical movements consist of several periodic local constrictions forming segments of small intestine. These movements help in mixing food with digestive juices and bringing the food intimately in contact with the mucosa.
- Pendulum movements consist of constrictions that move forward or backward for short distances moving the food over short distance in the small intestine.
- The chemical digestion of food in the small intestine is caused by the enzymes present in intestinal juice and pancreatic juice. The bile from liver poured into small intestine and assists splitting of fats.
- The micro-organisms present in the small intestine act on carbohydrates and proteins and hydrolyze them. These micro-organisms synthesize certain vitamins that are absorbed from there. These organisms also inhibit the growth of many harmful organisms and prevent infection.
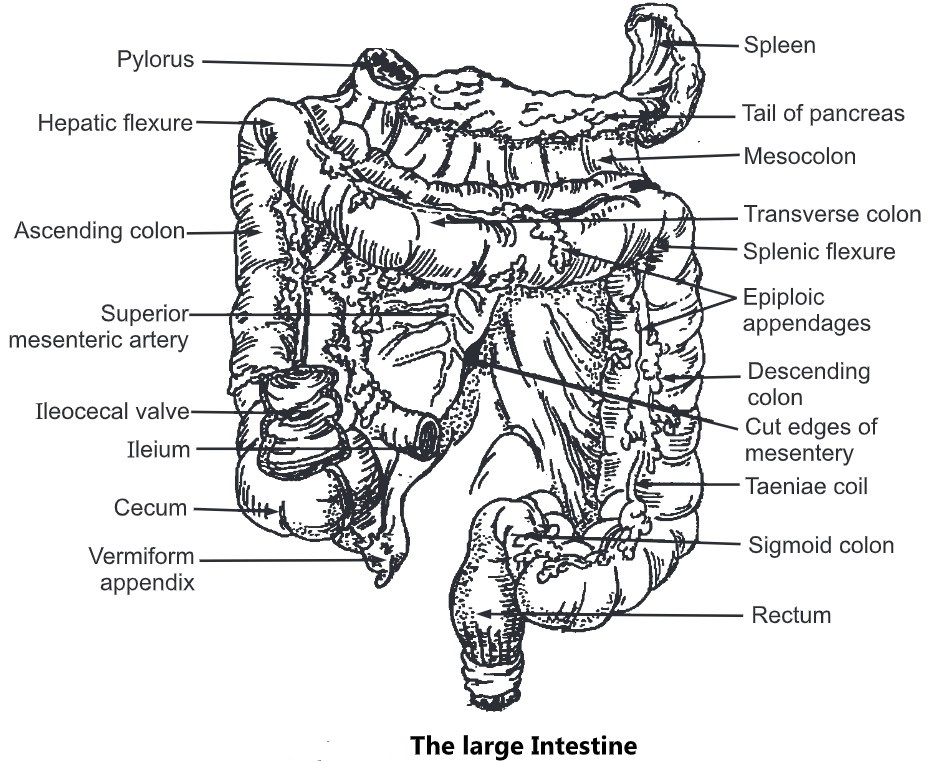
(6) Large Intestine (colon)
- It is about 01.5 metre long, starting from caecum in the right iliac fosse and terminating into rectum deep in the pelvis.
- Its lumen is larger than the small intestine. It surrounds the coiled up small intestine and is divided into different parts, ie. caecum, ascending colon, transverse colon, descending colon and sigmoid colon.
- Caecum is the first part of colon, and is a pouch like dilated portion which is blunt inferiorly and continues upwards as ascending colon.
- The small intestine opens into it and the opening is guarded by ileocaecal valve. A small narrow tube about 07 cm in length is attached to the end of caecum. This is known as appendix. Its functions are not known.
- The ascending colon is that part of colon which continues from caecum, passes upwards in the right side and on reaching liver bends to the left (hepatic flexure); to become the transverse colon.
- The transverse colon passes across the abdominal cavity from hepatic flexure on right side to the splenic flexure on left side. At splenic flexure (near spleen) it bends downwards to become the descending colon.
- The descending colon passes down the left side of the abdominal cavity and on reaching the left iliac region, it bends towards the right to enter into true pelvis.
- The descending colon on reaching the true pelvis, curves like the letter ‘S’ and hence named as sigmoid colon, which continues downwards as rectum.
- The four layers of tissues described in general plan are present in the large intestine. However, the longitudinal muscles in the muscle layer show typical arrangement.
- These muscles instead of forming a continuous layer, are arranged in three bands (05-06 mmthick), called as taeniae coli.
- These are located at regular intervals around the colon and are about one sixth shorter in length than the rest of the colon. This gives a puckered appearance to the colon. Another modification is found in mucous layer where the circular folds and villi are absent. It contains large number of goblet cells that secrete mucous and solitary lymph nodules.
Functions of Large Intestine
- Absorption of water: The contents entering the large intestine at caecum are fluid in consistency. Whereas the faeces are semi-solid which indicates that large amount of water is absorbed from large intestine. In addition, mineral salts and some drugs are also absorbed from large intestine.
- Microbial activity: Large numbers of micro-organisms are found in the large intestine. They include E. coli, E. aerogenes, S. faecalis, Cl. welchii etc. They synthesize Vitamin K and Folic acid.
- Defecation: When food enters into the stomach, it initiates a strong gastrocolic reflex. In response to this reflex, a strong peristaltic movement starts in transverse colon forcing its contents into descending and pelvic colon and into the rectum. Entry of contents in rectum stimulates stretch receptors in its wall, initiating the nerve impulses. These impulses are conveyed to consciousness and urge to defecate. As external anal sphincter is under conscious control, defecation can be inhibited until such time as it is convenient to defecate. Defecation involves strong peristaltic wave over the colon pushing the contents into the rectum, contraction of muscles of rectum, relaxation of internal anal sphincter and voluntary relaxation of external anal sphincter. Contraction of abdominal muscles and lowering of diaphragm increases the intra-abdominal pressure that helps the process of defecation.
(7) Rectum and Anus
- Rectum is a small dilated tube continuous with sigmoid colon above and to the anal canal below. It shows four layers of tissues as described in the general plan of alimentary canal. The mucous membrane shows large number of goblet cells which secrete mucous.
- The anal canal is about 03.8 cm long, and leads from rectum to the exterior. There are two sphincters that control the opening of anus, the internal anal sphincter consisting of involuntary muscles and the external anal sphincter of voluntary muscles.
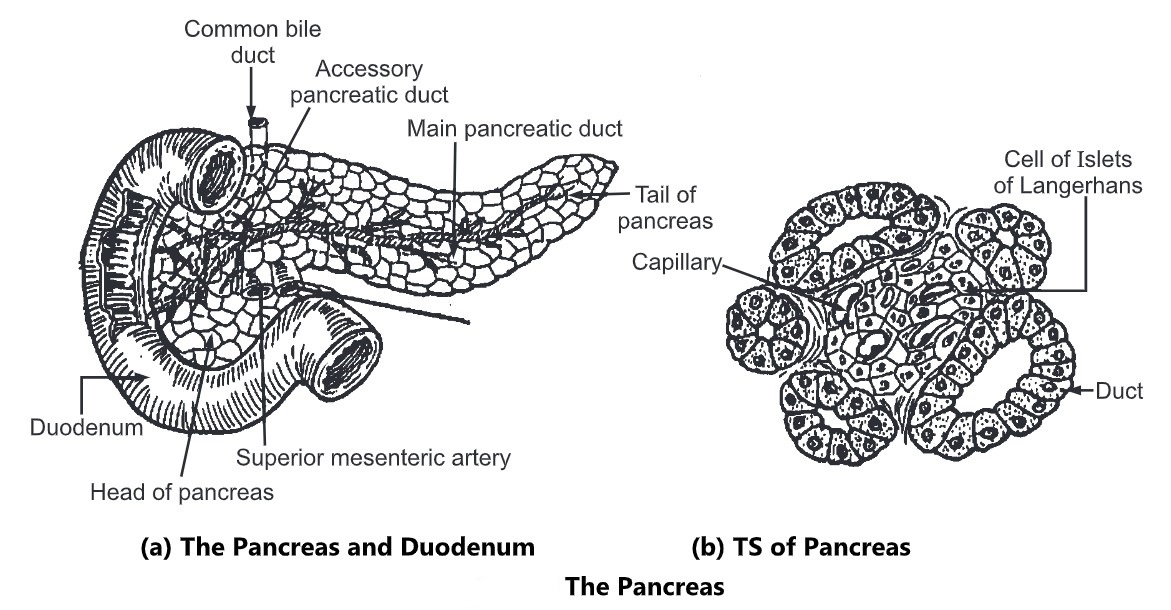
Pancreas
- It is a yellowish gray coloured gland situated in the epigastric and left hypochondriac regions of abdominal cavity at the level of first and second lumbar vertebrae. It is about 12-15 cm long with a broad head situated in the curve of duodenum, the middle part of the body situated behind the stomach and a tapering tail reaching to the spleen on the left side.
- It is a compound gland composed of large number of lobules. Each lobule is composed of many alveoli consisting of secretory cells. The lobule pours its secretions through a tiny duct into the pancreatic ducts; that extends the whole length of the gland and finally pours the secretions into the duodenum.
- The pancreatic duct before pouring its contents into duodenum; joins with common bile duct coming from liver. The union of these ducts form a dilated portion called ampulla of water.
- Opening of this ampulla in duodenum is controlled by the sphincter of oddi. Sometimes common bile duct and pancreatic duct open separately into the duodenum. The lobules are separated by a delicate connective tissue network. In this connective tissue, between the alveoli are found small groups of specialized cells. These are described as the Islets of Langerhans.
- They constitute the endocrine part of the gland, and secrete the hormones: insulin and glucagon that are directly poured into the blood.
Functions of Pancreas
The pancreas is both exocrine and the endocrine gland. The exocrine secretion of gland is pancreatic juice that is poured into the duodenum and contains enzymes that digest carbohydrates, proteins, and fats.
The composition of Pancreatic juice is as follows:
| Water Mineral salts Trypsinogen Chymotrypsinogen Amylase Lipase | About 600 — 800 ml of Pancreatic juice is produced per day. The pH of this juice is 8 — 8.4. |
The entry of acidic chime in the duodenum stimulates intestinal cells to secrete hormones; secreting, cholecytokinin, pancreozymin which in turn stimulates the secretion of pancreatic juice. The hormones secreted by the islets of Langerhans, and their role is described under
the Endocrine system.
Liver
- It is the largest gland in the body situated in the uppermost part of the abdominal cavity on the right side beneath the diaphragm.
- It weighs about 1500 grams and is irregular in shape. The upper surface is convex and lies beneath the diaphragm, while the under surface is irregular and is in contact with stomach, duodenum, right colic flexure of the colon and right kidney.
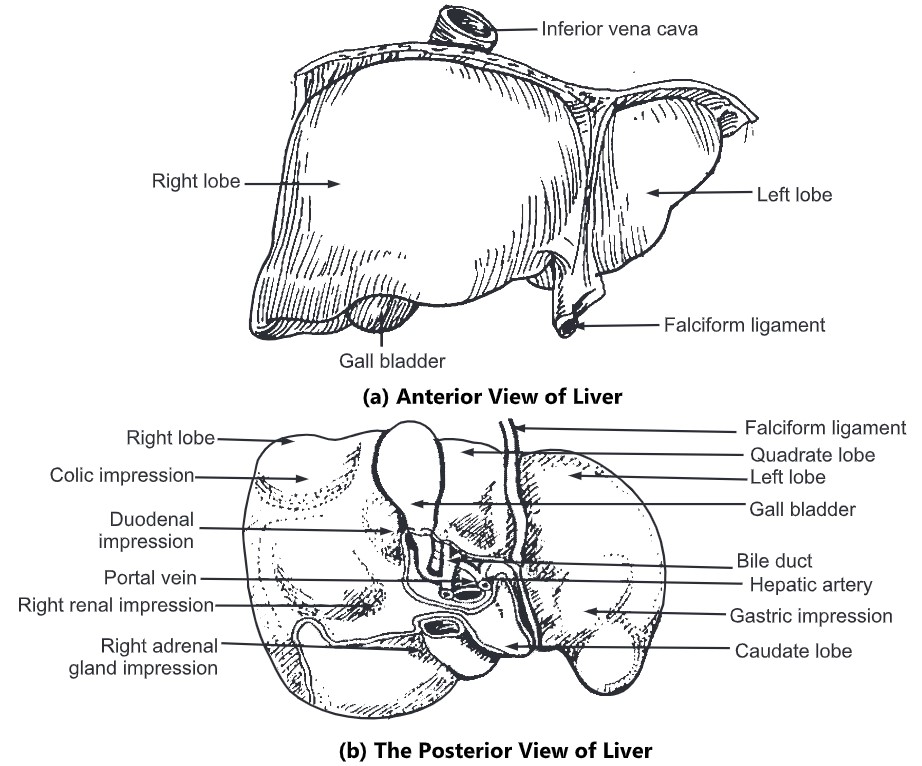
- It is enclosed in a thin capsule and partially covered by a layer of peritoneum. It is divided mainly into two lobes the right and left, however, the under surface of liver shows two more lobes; the quadrate lobe is the quadrilateral area between gall bladder and the fosse for the round ligament, and the caudate lobe is another quadrilateral area between inferior vena cava and the fosse for ligament venosum.
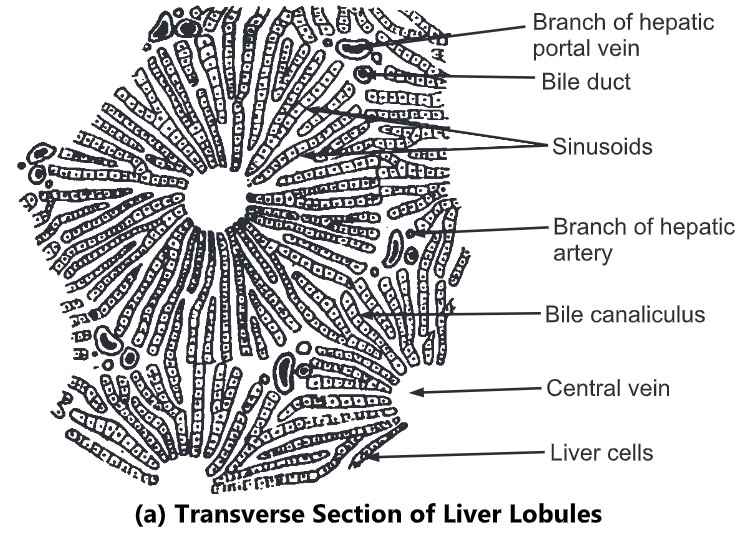
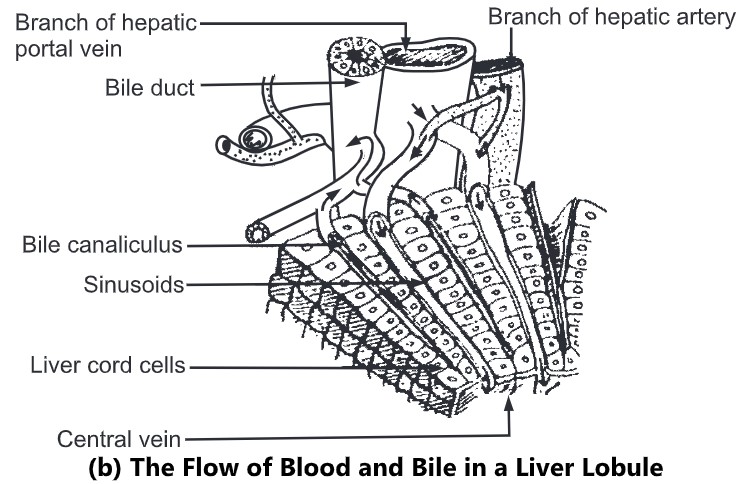
- Liver is made up of lobules which are polyhedral in shape. Each lobule is composed of cubical cells arranged radially, radiating from the central vein. Between two columns of cells there are sinusoids containing a mixture of blood from the tiny branches of the portal vein and the hepatic artery.
- Masses of such cells which form hepatic lobule (01 mm diameter) are separated from one another by connective tissue. Branches of portal vein, hepatic artery, and bile duct are enclosed in a tissue covering called as the ‘Gilson’s capsule’ which forms portal canal. Such portal canals are present surrounding the lobules.
- The blood from sinusoids comes in close contact with the liver cells. The sinusoids pour the blood into the vein in the centre of the lobule called as the interlobular vein. Interlobular veins from different lobules unite to form sublobular veins which in turn unite to form hepatic vein passing directly into the inferior vena cava.
- Bile is formed by the hepatic cells and is secreted into the fine bile canaliculi which commences between the columns of liver cells and carry bile to the periphery of hepatic lobule.
- The bile canaliculi join up to form larger bile canals until eventually they form the right and left hepatic ducts which drain bile from the liver. Thus, there is alternate arrangement of sinusoids (carrying blood) and bile canaliculi (carrying bile) in a lobule.
- Large bile ducts have lining of columnar epithelium and outer fibrous muscular tissue. By means of contraction of muscular layer bile is carried away. It is temporarily stored in the gall bladder.
Physiology of Liver
(1) Secretion of bile
Hepatic cells secrete an alkaline fluid called bile. It is composed of 90 per cent water, bile salts (sodium glycocholate, sodium taurocholate), bile pigments (bilirubin, biliverdin), cholesterol and mucin. Bile salts are helpful in digestion and absorption of fats. They reduce surface tension of fats and help in their emulsification. RBCs are destroyed in the liver and spleen. The haemoglobin of RBCs is broken down into globin and haem. Haem is again broken down into iron and porphyrins, which form bile pigments later on.
(2) Glycogenic functions
The portal vein carries the blood from the digestive tract which contains glucose and amino acids. It pours the blood into liver. The hepatic cells, by the action of enzymes, convert glucose into glycogen and it is then stored in liver. Whenever there is need of energy to body, the hepatic cells convert glycogen to glucose and pass it to the body cells through blood circulation. Thus, this glycogenic function helps to maintain the sugar level constant in the blood.
(3) Formation of urea
Portal vein carries blood containing amino acids to the liver. Hepatic cells by the action of their enzymes cause deamination of amino acids, i.e. amino group is set free which forms urea. Urea is carried away to kidneys by the blood and is given out of the body through urine.
(4) Denaturation of fats
The digested fats in the form of the fatty acids and glycerol are absorbed in the central lacteal duct. The fatty acids and glycerol again unite to form fats. This fat is carried away by the blood and is stored in the different tissues in saturated form. Whenever the energy is needed, this saturated stored fat is carried to the liver by blood. Then the hepatic cells cause the desaturation of this fat and pass to different tissues for utilisation.
(5) Functions related to blood
(a) Formation of RBCs in foetal life.
(b) Destruction of RBCs forming bile pigments and iron.
(c) Formation of plasma proteins, i.e. albumin and globulin.
(d) Formation of prothrombin and fibrinogen responsible for blood clotting.
(e) Formation of heparin, a natural anticoagulant in the blood.
(f) Storage of iron, vitamin B12.
(6) Maintenance of body temperature
The numerous chemical reactions occur in the liver, heat is generated which is helpful in maintaining body temperature.
(7) Excretion of toxic substances
The toxic substances entering the body through the alimentary canal are destroyed in the liver, e.g. alcohol, some drugs, etc.
As the liver is responsible for a number of intermediate metabolic reactions, it is called the chemical factory in the body.
Functions of the various organs and the physiology of digestion and absorption
The food is masticated or chewed by the teeth and moved around the mouth by the tongue and the muscles of the cheeks. It is mixed with saliva and formed into a soft mass or bolus ready for swallowing. The secretions of the salivary glands contain an enzyme ‘ptyalin’ which converts starches into maltose. The salivary secretion also moistens and lubricates the food. It also cleans the mouth and keeps the structures within the mouth soft and pliable. The bolus of food is pushed back into the pharynx by the upward movement of the tongue. The muscles of the pharynx further propel it down into the oesophagus. The presence of bolus in the pharynx stimulates a wave of peristalsis and propels the bolus through the oesophagus to the stomach. The walls of the oesophagus are lubricated by mucous which assists the passage of the bolus during peristaltic contraction of the muscular wall.
The stomach acts as a temporary reservoir for food thus allowing the digestive juices to act on food. It also produces gastric juice which contains water, mineral salts, mucous, hydrochloric acid, enzymes, i.e., pepsinogen, renin and the intrinsic factor. Water in the gastric juice further liquefies the swallowed food. Hydrochloric acid acidifies the food and stops the action of salivary ptyalin. It also converts pepsinogen to the active enzyme pepsin and kills many microbes which may be harmful to the body. Pepsin converts proteins into peptones, and renin changes soluble caseinogens from the milk to insoluble casein which in turn is converted by pepsin into peptones. Renin is present in gastric juice of infants only. The intrinsic factor is necessary for the absorption of vitamin By. The mucous in the gastric juice prevents mechanical injury to the stomach wall by lubricating the contents. It also prevents chemical injury by acting as a barrier between the stomach wall and other constituents of gastric juice. Muscular action of the stomach mixes the food with gastric juice and moves it to the small intestine. Absorption takes place in the stomach and to limited extent water, glucose, alcohol and some drugs are absorbed through the walls of the stomach into the venous circulation.
The small intestine further progresses the movement of its contents by its peristaltic, segmental and pendulum movements; besides it secretes intestinal juice which consists of water, mucous and various enzymes. The intestinal juice is alkaline in nature. The enzymes in the intestinal juice perform various functions. Enteropeptidase converts inactive pancreatic trypsinogen and chymotrypsinogen to active trypsin and chymotrypsin which further convert peptones into peptides and polypeptides. Intestinal and pancreatic amylase convert polysaccharides to disaccharides. Peptidases convert peptides and polypeptides into amino acids. Lipase converts fats into fatty acids and glycerol. Sucrose, maltase and lactase act on corresponding disaccharides to convert them into monosaccharides. The intestinal juice thus completes digestion of carbohydrates, proteins and fats. The solitary lymph follicles and aggregated lymph follicles in the villi of small intestine help in protection against infection by micro-organisms. All the digested materials are also absorbed in the small intestine.
The end products of digestion of carbohydrates, proteins and fats are monosaccharides (mainly glucose), amino acids, fatty acids and glycerol respectively. Glucose is absorbed into the capillaries of the villi and transported in the portal circulation to the liver. Amino acids also follow the same path. Fatty acids and glycerol are absorbed into the lacteals of the villi and are transported via, the thoracic duct to the left subclavian vein. Then they are carried to the liver where they are reorganized and recombined.
The food passing through the small intestine enters the large intestine. In the large intestine, absorption of water continues till semi-solid consistency is achieved. Mineral salts and some drugs are also absorbed into the blood capillaries from the large intestine. The large intestine exhibits a wave of strong peristalsis only at long intervals. This forces its contents into the descending and pelvic colon and finally to the anus.
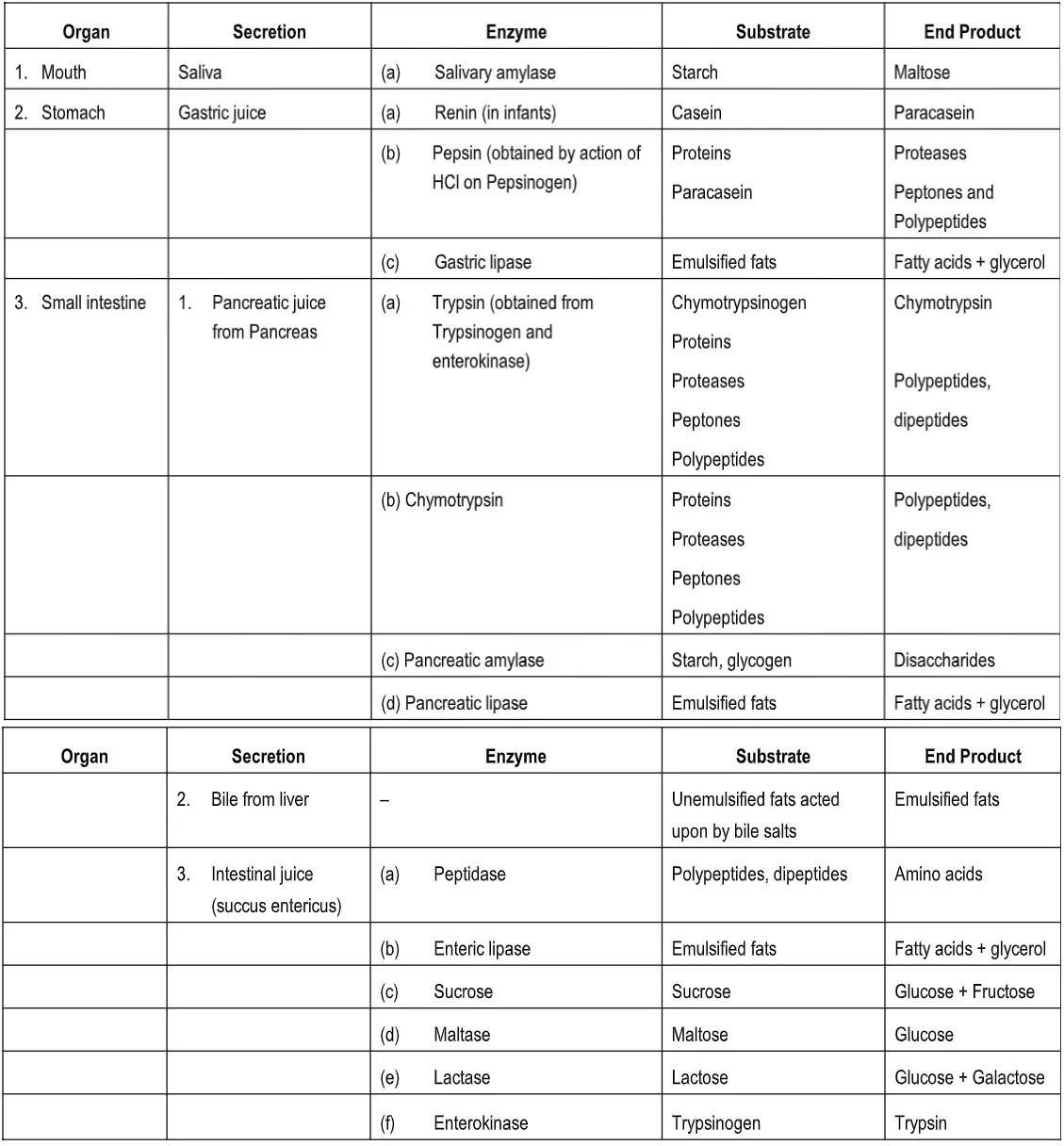
Table: Digestion of food in the alimentary canal