Contents:
Components of Blood
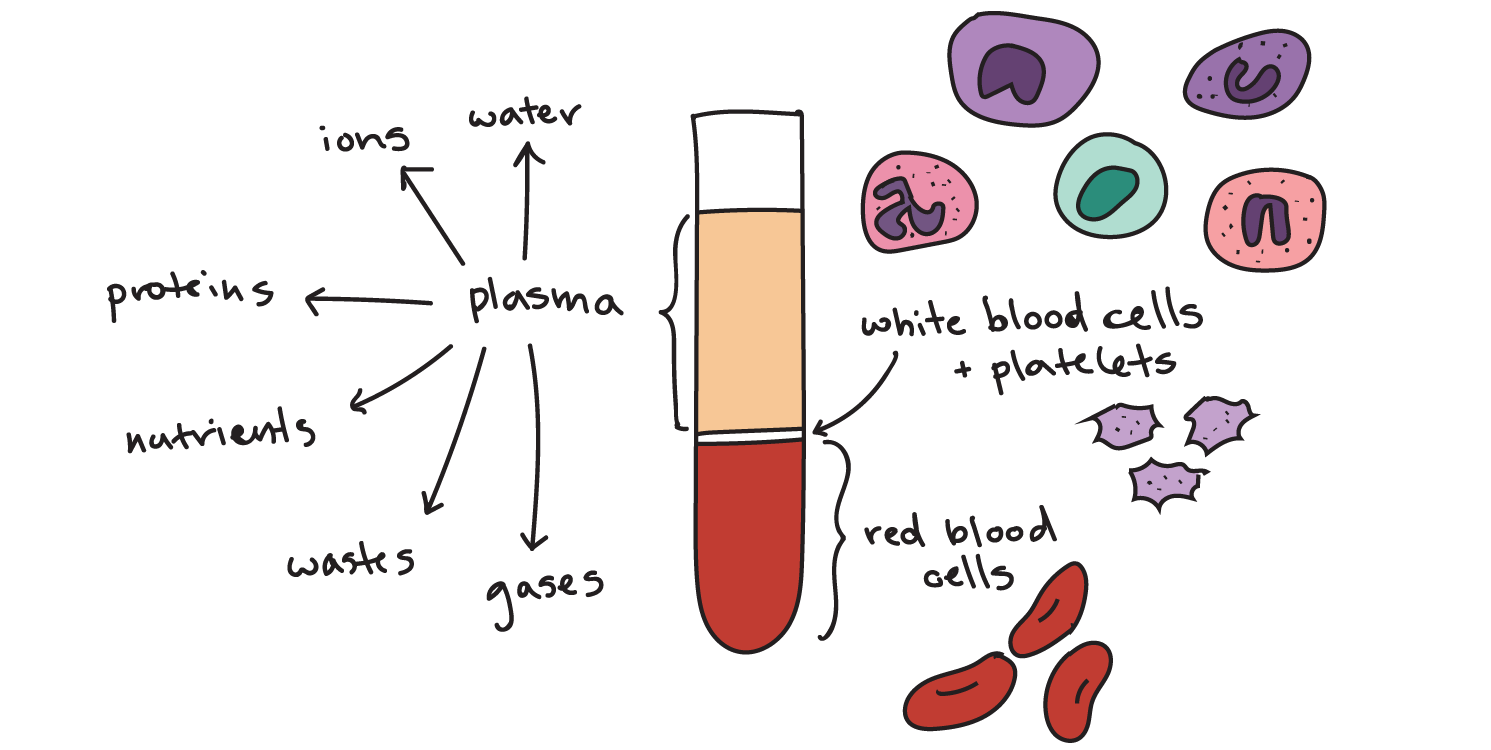
A 75 kg human has about 4 liters of blood, comprising about 8% of body weight. About 60% of blood is plasma, made up of 90% water, while the remaining 40% of blood is cells and thrombocytes.
What is blood?
-
Plasma is the main component of blood and consists mostly of water, with proteins, ions, nutrients, and wastes mixed in.
-
Red blood cells are responsible for carrying oxygen and carbon dioxide.
-
White blood cells are part of the immune system and function in the immune response.
- Platelets are responsible for blood clotting.
1. Plasma
With the exception of oxygen and carbon dioxide carried by hemoglobin, most food, waste, defense, and messenger molecules are carried in solution in the plasma. Plasma also contains plasma proteins, the main ones being:
- albumins which maintain a high colloidal osmotic pressure in plasma and can bind and carry some hormones: about 60% of plasma proteins are albumins;
- fibrinogen (4%) which is made in the liver and is important for blood clotting;
- globulins (36%) of which there are three types, α, β, and γ. α-globulins and β-globulins are made in the liver and transport fats and fat-soluble vitamins in the blood: low-density lipoprotein transports cholesterol from the liver to body cells; high-density lipoprotein helps to remove cholesterol from arteries. γ-globulins are immunoglobulins (antibodies). Plasma also contains some vitamins, hormones, and enzymes (especially concerned with blood clotting), and antimicrobial peptides. Plasma electrolytes are inorganic compounds that have ionized in solution. The major cation is Na+ which has an important effect on fluid movements and helps to determine fluid volume; the main anion is Cl–. Among other important ions are K+, Ca2+, Mg2+, and PO4 3–.
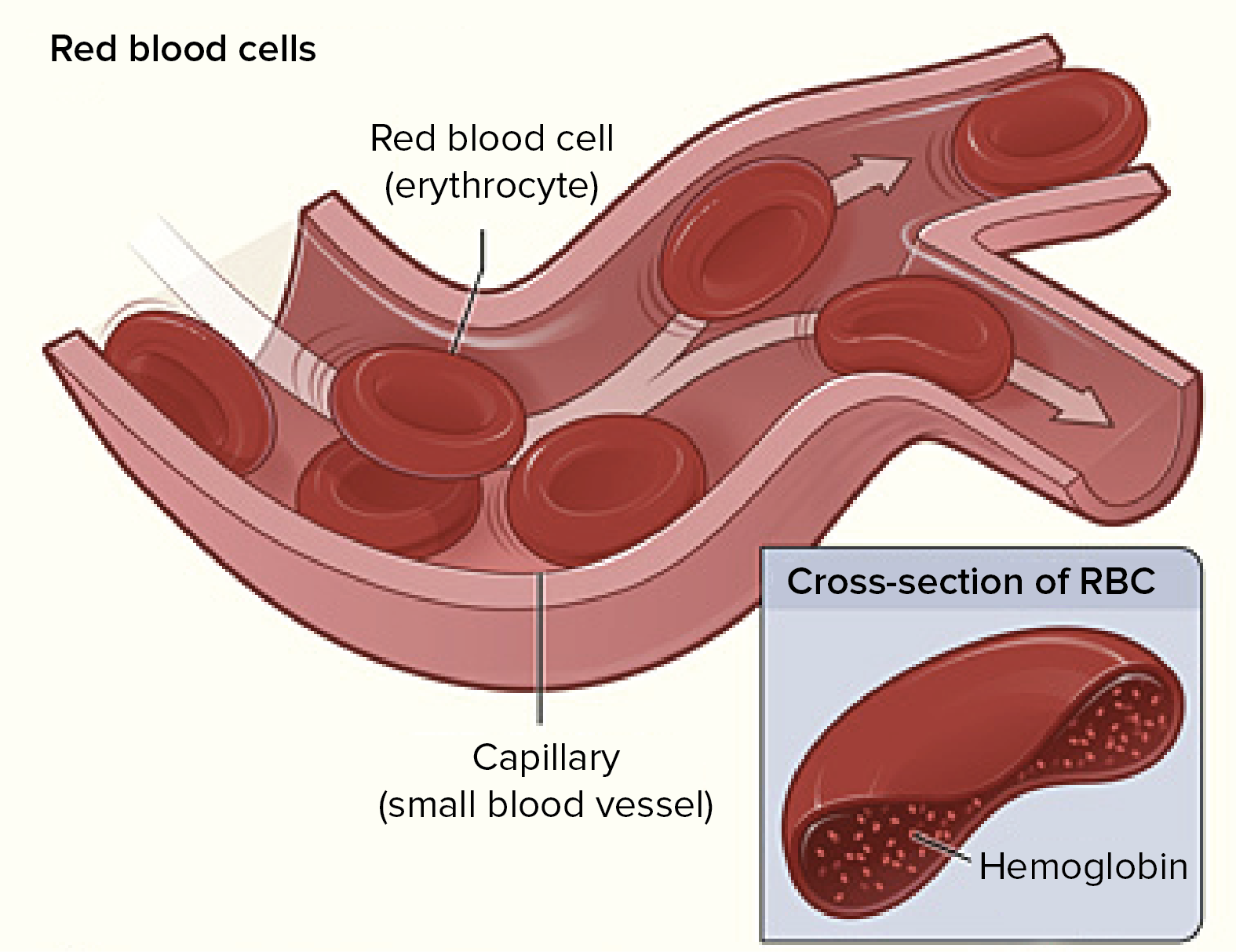
2. Red blood cells (erythrocytes)
Red cells make up about 40% of the human blood volume (this is known as the hematocrit or packed cell volume, strictly including all blood cells). Humans possess 25 × 1012 red cells, each cubic millimeter of blood having 5.5 million red cells (men) or 4.8 million red cells (women). Red cells are biconcave disks, 7 μm in diameter and 2 μm thick, with a large surface area for diffusion. Mature red cells are made up virtually entirely of hemoglobin: the red cell loses its nucleus and most of its organelles. The thin, strong, flexible, semi-permeable cell membrane facilitates movement through vessels.
Red cell production (erythropoiesis)
- In the fetus, red cells are made successively in the yolk-sac, liver, and spleen, and (at over 4 months gestation) in the bone marrow where they are also made in the child and the adult.
- They start life as stem cells, undergoing a series of divisions during which the nucleus gets smaller and disappears after several divisions: the resulting reticulocyte enters the bloodstream.
- The extensive endoplasmic reticulum which characterizes the reticulocyte is lost, and the mature erythrocyte, the definitive red cell, is the result.
- Adult erythropoiesis makes 1010 cells per hour (enough for 440 ml per week, ‘one pint). The process requires amino acids, iron, and vitamins (folic acid, riboflavin, B6, and B12).
- The controller of erythropoiesis is the glycoprotein hormone erythropoietin, synthesized by kidney cells sensitive to reduced oxygen tensions in the blood.
- After about 120 days, red cells become leaky and senescent: they are destroyed by splenic macrophages. Amino acids and iron are recycled, the rest of the heme ends up as bile pigments.
3. White blood cells (leukocytes)
White cells are divisible into granulocytes and agranulocytes. White cells are nucleated and can migrate through vessel walls. Their metabolism is more complex than that of red cells and they can synthesize proteins. There are between 4 and 6 × 103 white cells per mm3, although this can increase by over fourfold following infection or in certain diseases.
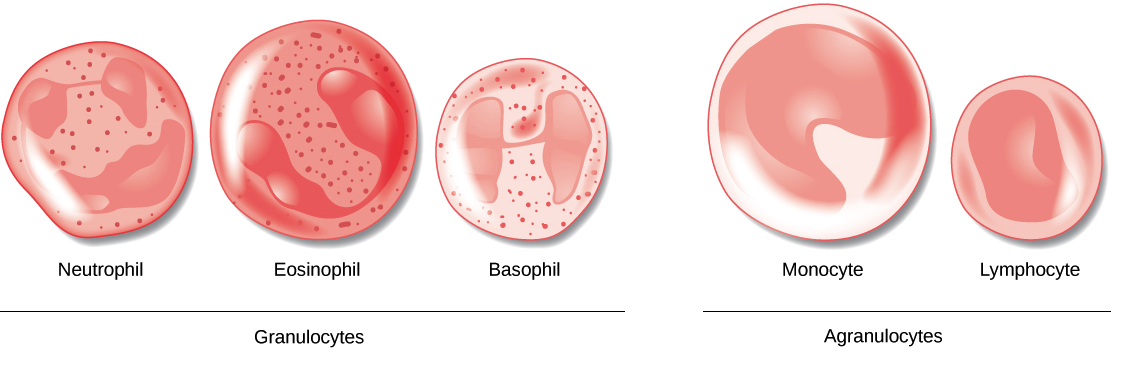
Granulocytes
- Neutrophils (‘polymorphs’) are scavenger cells with lobed nuclei which engulf and destroy microorganisms, etc., using an armory of lysosome-derived enzymes. They are the most frequent white cell seen in a blood smear.
- Eosinophils phagocytose antigen-antibody complexes and counteract basophil degranulation products.
- Basophils contain histamine and other vasoactive amines. When IgE antibody combines with antigen, the basophil (mast cell in tissue) degranulates, releasing the amines and causing inflammation, etc. They are seen in anaphylactic hypersensitivities such as asthma and hay fever.
Granulocytes develop in the bone marrow from stem cells via myeloblasts: about 100 million neutrophils can be produced per day, with a lifespan of about 1 week.
Agranulocytes
- Monocytes (mobile macrophages) have large folded nuclei and fine cytoplasmic granules. They originate from stem cells through monoblasts in the bone marrow, and enter the bloodstream for 30–70 hours, before leaving it. In tissue spaces, they enlarge to form macrophages, which are important in the liver, lungs, and lymphoid organs for ingesting foreign particles in order to destroy them or to present them to lymphocytes.
- Lymphocytes are small, nonphagocytic cells with large nuclei. They are concerned principally with adaptive immunity.
4. Thrombocytes (platelets) and hemostasis
- Blood clotting is a complex phenomenon requiring thrombocytes (platelets) and at least 15 clotting factors present in the bloodstream or on cell membranes.
- Thrombocytes are colorless, ovoid disks, smaller than red cells, derived from fragmented meta megakaryocytes, derived in turn from bone marrow stem cells; production is under the control of thrombopoietin.
- Platelets are effectively anucleate packets of chemicals needed to initiate clotting of blood and plugging of leaks.
- The clotting process begins when plasma encounters a rough surface or a protein tissue factor found on the outer surface of many cell types, but not on the endothelial cells lining blood vessels.
- When tissue factor reacts with a specific circulating plasma protein, for example when a blood vessel is damaged, a cascade of chemical reactions is triggered.
- In such a cascade, the product of each step of the reaction series acts as a catalyst for the next step, and the molecules involved are, like enzymes, re-used many times. Thus the number of molecules is amplified at each step in the series.
- Ultimately, thromboplastin is activated. Thromboplastin acts to convert prothrombin (a plasma protein produced by the liver) to the enzyme thrombin.
![]()
Thrombin then converts fibrinogen, a soluble plasma protein, to fibrin.
![]()
- The fibrin molecules clump together to form an insoluble mesh which traps blood cells to form a clot.
- The clot contracts, pulling together the wound edges. (Clotting also occurs if blood is put in a glass tube, apparently triggered by contact with the glass. The clear fluid remaining above the clot is serum.)
- The autonomic nervous system (through its sympathetic fibers) helps to control the loss of blood. When about 10% of the blood is lost, the blood pressure suddenly falls and the body enters a state of shock.
- Reflexes are triggered leading to artery and vein vasoconstriction; the renin/angiotensin system also facilitates vasoconstriction; tachycardia (rapid heart rate) may compensate for reduced blood pressure, delivering extra blood to the brain and heart.
- This can allow short-term survival if even 40% of the blood volume is lost. Deficiencies in various clotting factors can lead to failures in the clotting mechanisms: hemophilia is a well-known example: in the most common form, there is a congenital absence of Factor VIII which activates prothrombin.
- Anticoagulants circulate in the blood to prevent dangerous, unwanted clots: one of the most powerful is the polysaccharide heparin produced by basophils. Clot destruction is facilitated by fibrinolysis, a process by which plasmin digests fibrin.
You May Like: Cells of the Immune System
Human blood groups
ABO system
If red blood cells from one person are mixed with plasma from another, agglutination of red cells may occur due to isohemagglutinins (IgM antibodies) of the ABO blood group system. The relevant antigens are A and B (derived from sugar, H substance) on red cells. The antibodies may derive from reactions to dietary sugars or to polysaccharides on the surfaces of gut microflora. There are four blood groups; people in:
- group O has neither A nor B antigen
- group A have A antigen
- group B has the B antigen
- group AB has both antigens
- group O have anti-A and anti-B antibody
- group A has an anti-B antibody
- group B have an anti-A antibody
- group AB has neither antibody
People in group O are known as ‘universal donors’ as they can give blood to any recipient, and those in group AB are known as ’universal recipients’ as they can receive blood from any donor, with respect to the ABO system.
Rhesus system
- Most people have the D antigen on their red cells: they are Rhesus positive (Rh+); the rest are Rh–. If an Rh- mother has a Rh+ baby (the gene for D being inherited from the Rh+ father) there are usually no problems with the first pregnancy, but the mother will probably be immunized against the baby’s D antigens because of bleeding at birth.
- IgG antibodies to D are made: these can cross the placenta. Thus a second or subsequent Rh+ baby is at risk from anti-D antibodies which cross the placenta and destroy the fetus’ red cells, leading to hemolytic disease of the newborn.
- Treatment is to give Rh– mothers passive anti-D antibody immediately after birth; this destroys any Rh+ red cells from the baby’s blood before they can immunize the mother.
- There is less problematic if the mother and father are ABO incompatible: if the father and baby are, for example, of blood group A and the mother is of blood group O, the mother’s anti-A antibodies will destroy the baby’s A, Rh+ blood cells before the D antigen can immunize the mother.