Contents:
The hepatitis A virus is spread via the fecal-oral route from person to person mainly through the consumption of infected food or drink and/or contact with infectious persons. Symptoms range from asymptomatic inflammation to fulminant hepatitis. It is possible to transfer HAV via oral-anal intercourse as well. Hepatitis A, also called hep A, is a contagious liver infection caused by the hepatitis A virus.
The History of Virus Discovery
The viral etiology of outbreak jaundice was not generally recognized by doctors until the middle of the twentieth century. J. Dunlop, G. Findlay, and H. Brown’s results, published in 1931, indicated a virus as the most likely etiological agent of the “catarrhal jaundice” known earlier. Later, this clinical condition was known as hepatitis A disorder.
In 1973, the Hepatitis A virus was detected by S.M. Feinstone and colleagues from immune electron microscopy results for patient feces.
Classification
Hepatitis A virus (HAV) pertains to the Picornaviridae family.
Despite the fact that HAV shares certain essential characteristics with other picornavirus genera, it is very distinct and is known as the only species in the Hepatovirus family. There are strains that infect non-human primates (three genotypes) spontaneously occurring, as well as four genotypes containing human-infectious viruses. There is only one serotype known.
Structure of Virus
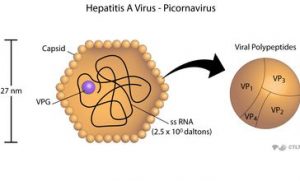
HAV, containing a linear single-stranded (+) RNA genome, is a 27-32 nm spherical particle of icosahedral symmetry. Its genome is a single-stranded RNA molecule of the positive-strand polarity of 7478 bases. This sequence codes for a polyprotein which is processed to give rise to viral proteins VP-1, VP-2, VP-3, and others. Intact virions have an RNA nucleocapsid, a covalently bound VPg protein
Virion resistance
HAV shows enhanced stability in virions. It is resistant to ether and acid therapy ( e.g., pH 1.0 for 2 hours) as well as heating (60 ° C for 10 hours). It stays viable for months beyond the host. The virus is killed through UV irradiation, by autoclaving, by boiling for 5 minutes in water, and by treating with formaldehyde or disinfectants including chlorine.
Viral Replication Cycle
- The proliferation of HAV is believed to be limited to hepatocytes and epithelial gastrointestinal cells. For other picornaviruses, viral replication is identical.
- Genomic (+) RNA translation with the development of structural and non-structural proteins, including RNA polymerase, is accompanied by uncoating.
- It replicates the viral RNA genome through an intermediate negative strand. From the genomic positive RNA strand, viral proteins are further developed.
- In bile and blood, virus particles emerge, being released predominantly into the biliary canaliculus via the apical hepatocyte membrane and into the bloodstream through the basolateral membrane.
- The process of viral release and secretion is not yet understood, but hepatocyte necrosis is not commonly followed.
Pathogenesis, Clinical Findings and Immunity of Hepatitis A
- An ill individual is the cause of the infection. This disorder primarily affects children or young adults.
- Transmission of hepatitis A occurs through a fecal-oral path (waterborne and foodborne infection) and through direct interaction.
- The time of incubation lasts from 10-50 days (average about 1 month).
- In enterocytes and in area lymph nodes, primary virus replication occurs. HAV comes into the blood at the end of the incubation cycle, resulting in viremia. Viruses join hepatocytes directly from the portal vein or from the systemic bloodstream.
- Enterohepatic cycling is observed with HAV. The viruses are secreted into the bile after replication inside hepatocytes with eventual excretion by feces. Otherwise, the next reabsorption would take place in the gut. The latter results in hepatic cells repeating viral uptake. Before specific antibodies kill viruses, the enterohepatic cycle begins.
- The onset of the condition is accompanied by fever, jaundice, bilirubin, and elevation of aminotransferase.
- An acute HAV infection is most frequently asymptomatic in small children. In comparison, the clinical symptoms of older children and adults vary from minor inflammation to potentially lethal fulminant hepatic disease.
- However, complete healing occurs in most cases of hepatitis A; chronicity is not noted.
- Both humoral and cellular immunity are activated by HAV infection.
- Antibodies directed toward HAV proteins are caused by IgM, IgG, and IgA and can typically be recognized by the onset of clinical symptoms. They neutralize the behavior of viruses, promoting recuperation.
- Cell-mediated immunity, on the other hand, induces immune-mediated damage of hepatocytes, aggravating hepatic inflammation.
- The lifetime defense against HAV infection is provided by post-infectious IgG-mediated humoral immunity.
Laboratory Diagnosis of HAV Infection
- A liver biopsy permits a diagnosis of hepatitis A in the tissue. Scientific, pathological, and epidemiological findings are accompanied by tests for impaired liver activity, such as serum alanine aminotransferase ( ALT) and bilirubin.
- HAV can be characterized by multiple immunoassays (immunofluorescence test, ELISA), nucleic acid hybridization assays, or PCR in particular clinical specimens (liver biopsy, stool, bile, or blood).
- About 1-2 weeks prior to the first liver enzyme abnormalities, peak virus levels are observed in the feces.
- In fecal samples of hepatitis A patients, virus particles are observed by immune electron microscopy. The infection emerges early in the disease and dies just two weeks after jaundice starts.
- Serological diagnosis is more important for use in hospitals.
- Anti-HAV antibodies emerge in the IgM fraction, peaking around 2 weeks after liver enzyme elevation. Anti-HAV IgG antibodies monitor disease initiation and survive for decades to come.
- The identification of IgM anti-HAV antibodies in the blood thus supports the 99% accuracy of the hepatitis A diagnosis. For testing HAV antibodies, ELISA is the tool of choice.
Principles of Hepatitis A Treatment and Prophylaxis
- There is no need for treatment of subclinical and minor cases of viral hepatitis A. Manifested case care is supportive, precise antiviral therapies are not available.
- Human immunoglobulin can be provided for passive prophylaxis of exposed individuals.
- Various culturally inactivated vaccines are widely used for complex prophylaxis. Between 18 and 24 months, infants are immunized annually.
- Antibodies caused by vaccines are long-lasting and survive for at least 20 years. Vaccination gives long-term security from HAV; it is now possible to prevent this virus in the future.
