Arteries
The arteries are efferent vessels that take blood to the capillary beds away from the nucleus. Both vessels, except the pulmonary arteries, contain oxygenated blood in adults: deoxygenated blood is transported from the heart to the lungs by the pulmonary arteries. The aorta from the left ventricle (carrying blood to the body in the systemic circulation) and the pulmonary trunk from the right ventricle are the great arteries arising from the heart.
Arteries are made up of the following.
- Tunica intima: the innermost, smooth, lining endothelium; connective tissue; elastic tissue.
- Tunica media: thick connective and elastic tissue and smooth muscle (more muscle in arterioles, the more connective tissue in great arteries).
- Tunica adventitia: collagen fibers and smooth muscles, with nerves, lymphatics, and small blood vessels.
During systole (the ventricular contraction phase), the elastic walls of the large arteries make adjustments to high pressure; the pulmonary arteries are oval in cross-section, helping to damp blood surges from the right ventricle and thereby shielding the capillary beds of the alveoli of the lungs. With extensive smooth muscles supplied with autonomic nerve fibers, arteries branch to form arterioles: they can either constrict or dilate and act as ‘stopcocks’ regulating blood supply to capillary beds (by ≤400%).
Capillaries
On the ends of the finest arterioles, capillaries are located that connect the arterial and venous networks. They have only a single layer of endothelial cells on their walls. The approximate length of the capillaries of an adult individual is measured at 96 000 km, giving an immense surface area for the trade of gas, food, and waste. There are three capillary types:
- continuous capillaries in muscle cells;
- Fenestrated capillaries in the kidneys and endocrine glands (with pores between adjacent endothelial cells)
- Sinusoids (discontinuous capillaries) with membrane-covered openings between hepatic and spleen endothelial cells.
Capillary blood flow
- Blood leaves the heart pumping at 30-40 cm sec-1 but slows in arterioles to 2.5 cm sec-1 and in capillaries to less than 1 mm sec-1, where it persists for a few seconds as there is an exchange of gas and nutrients: the single-cell endothelium allows small molecules to move through while maintaining large molecules and cells.
- At the arteriolar end of the capillary, hydrostatic arterial blood flow pushes water and small solutes into the spaces of tissue fluid. At the venous end of the capillary, the colloidal osmotic pressure of the plasma proteins draws water and tiny solutes back into the blood through osmosis: the lymphatic system drains all non-resorbed material.
Veins
- Venules drain capillaries, uniting small venules to form veins. For the drawing back of tissue fluid into the blood circulatory system, the smallest venules are important.
- The veins drain deoxygenated blood to the right atrium of the heart from the venules (the venae cavae from the large veins). Oxygenated blood from the lungs to the left atrium is drawn by the pulmonary veins; blood from the capillaries of the gut to the capillaries of the liver is taken by the hepatic portal vein.
- Veins contain the same layers of tissue as arteries, but the tunica media is much thinner and the walls have less elastic tissue and muscle: thus, veins are very compressible and distensible.
- In order to stop blood back-flow, they have semi-lunar valves. Venous pressure is minimal, but the flow is assisted in exercise by massaging body muscles.
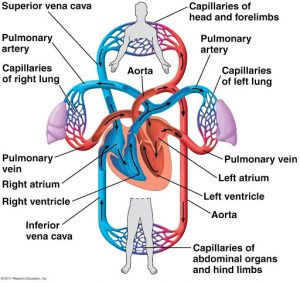
Circulatory patterns
- The umbilical cord includes the umbilical vein that holds oxygenated blood from the placenta (where there is an exchange of nutrients and gases between maternal blood and fetal blood in the capillaries: no mixture of blood) to the fetal abdomen before birth (in the fetus).
- The vein divides here: some blood goes to the liver, much of it bypasses the liver (through the ductus venosus) and enters the inferior vena cava, combining fetal tissue with deoxygenated blood.
- The vena cava opens into an atrium on the right. Approximately 67 percent of the blood moves via the foramen ovale, straight to the left atrium and thus out through the left ventricle and aorta.
- Blood discharges into the right atrium from the head: much of this flow to the right ventricle and pulmonary arteries, but the ductus arteriosus short-circuits the lungs so that blood flows straight to the aorta from the pulmonary arteries; about 10% of blood from the pulmonary artery travels to the forming lungs.
- At birth, as the baby takes his / her first breath, the lungs inflate under adrenaline (epinephrine)/shock stimuli, the pulmonary arteries become completely functioning, the pressure on the right side of the heart decreases, and the flap over the foramen ovale closes as the differential right-left heart pressure reverses. The ductus arteriosus coils and forms a ligamentous strand later; if the cord is severed, the umbilical arteries atrophy.
After birth the pattern is as follows: left heart–>body–>right heart–>lungs–>left heart.
Blood pressure
Arterial blood is pushed with tremendous force by ventricular contraction: blood pressure tests the force per unit area by which blood presses against vessel walls. Natural adult human arterial blood pressure, measured in the upper arm, as the ventricles contract (systole), is around 120 mm mercury (Hg) and 80 mm Hg when they relax (diastole): this is written as 120/80.
Blood pressure is determined by:
- strength and rate of heart contraction
- the elasticity of arterial walls
- rate of blood flow.
The blood flow rate is directly proportional to the pressure it bears. The flow of fluid in a tube is proportional (where r = radius) to r 4. Smooth muscle contraction or relaxation will change the diameter (2r) of the arterioles, thereby deeply influencing flow rates. The muscles thus maintain power under the influence of autonomic nerves and chemicals such as adrenaline (epinephrine).
Arteriolar constriction and dilation control flow as needed: in exercise, flow to muscles increases, digestion to the gut, and when hot to the skin. It is necessary to provide continuous blood flow to the brain (fainting induces a reduction such that the force of gravity does not have to be overcome in order to bring blood to the brain; the blood supply is thus protected). Blood flow may be affected by elevated brain activity: turning pale with anxiety or frustration, blushing with shame, penis/clitoris erection with sexual arousal.
References
https://books.google.com/books?id=i9YwWhkHOs4C