Contents:
Introduction
For body cells to function effectively, their environment should be maintained relatively constant (homeostasis). Continuous working of cells necessitates utilization of nutrients (glucose) and oxygen and results in the production of certain waste substances. Thus, the concentration of substances present in the internal environment of the body (extracellular fluid) varies. To avoid such variations and to maintain homeostasis, the waste products of cell metabolism should be removed from the body. Amongst the body systems involved in maintaining homeostasis are the digestive system, respiratory system, skin, and urinary system. The urinary system is, however, the main system maintaining the homeostasis of the internal environment. It eliminates the variety of cellular metabolic products such as urea, uric acid, and creatinine and maintains the water and electrolyte balance of the body.
Following are the main excretory organs in the human body:
Kidneys
- They excrete water, inorganic salts, and nitrogenous wastes from protein catabolism.
- Lungs: They excrete carbon dioxide, water vapor.
- Skin: It excretes heat, water, carbon dioxide, salts, and urea.
- Alimentary canal: It excretes undigested waste, water, salts, and heat.
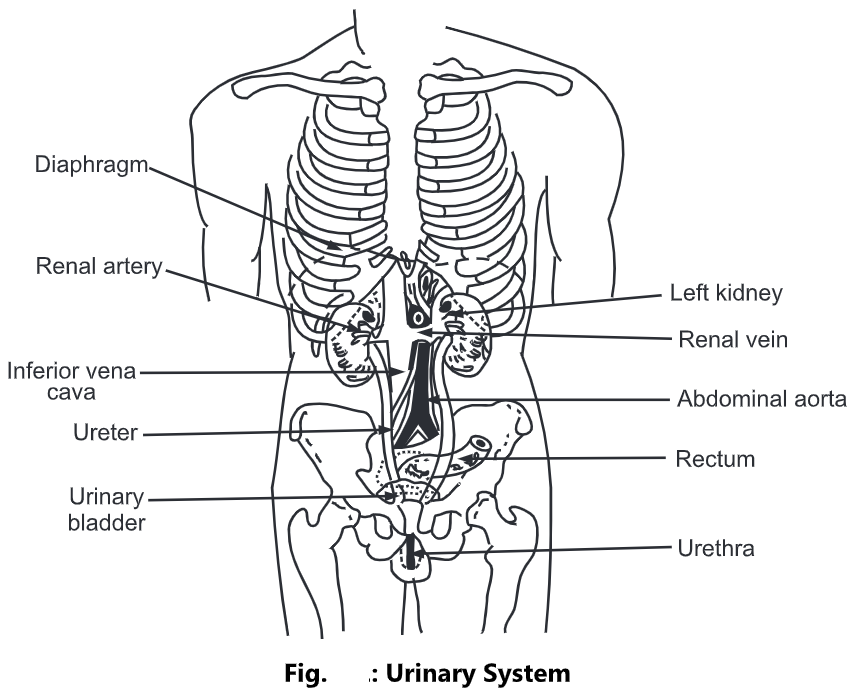
- Two kidneys, two ureters, one urinary bladder, and one urethra constitute the urinary system. The kidneys form the urine, which passes through the ureter to the bladder for excretion.
- This helps in maintaining the fluid and electrolyte balance and disposal of waste material from the body.
- The ureter propels urine from the kidneys into the bladder by peristaltic contraction of their muscular walls.
- Peristalsis is stimulated by the presence of urine. The urinary bladder acts as a reservoir of urine.
- The accumulated urine is excreted through the urethral opening. The urethra is longer in males and short in females.
- Kidneys are bean-shaped organs located on the posterior abdominal wall, behind the peritoneum, and one on each side of the vertebral column.
- Their location is at the level of the twelfth thoracic vertebra above the third lumbar vertebra. The right kidney is a little lower than the left because of the presence of a bigger right liver lobe.
- Each adult kidney measures about 12 cm in length, about 07.5 cm in width, and about 02.5 cm thick.
- Each kidney is covered by a thin smooth fibrous coat called the renal capsule. A mass of adipose tissue surrounds the renal capsule that helps to hold the kidney firmly in place and is called an adipose capsule.
- The outermost covering over the adipose capsule is a layer of dense irregular connective tissue called renal fascia. The renal fascia anchors the kidney to the posterior abdominal wall.
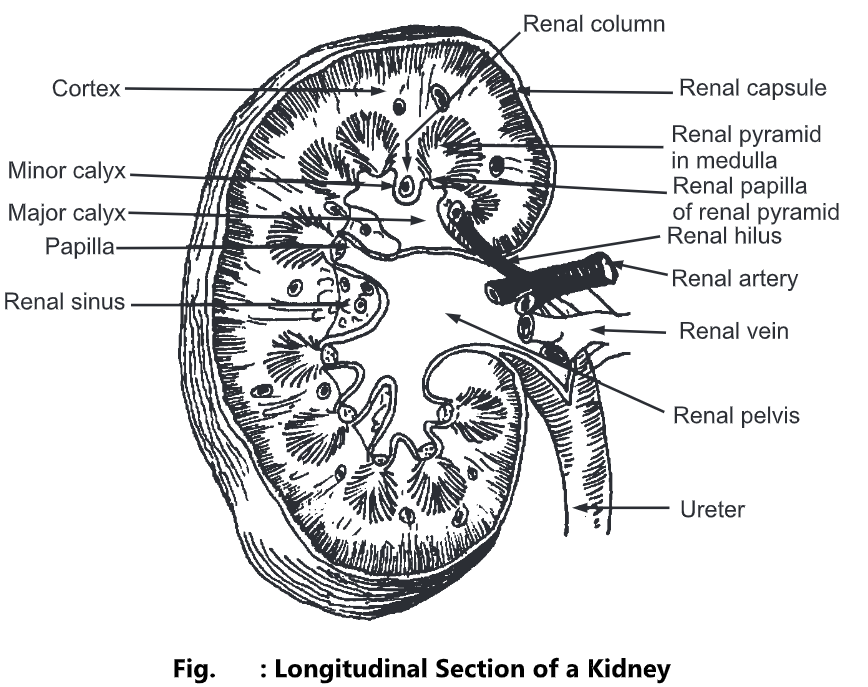
- LS of kidney shows the convex border on the lateral side and the concave facing medially. In the center of the concave medial surface, there is an indentation (notch) called the renal hilum.
- Through the hilum, the renal artery enters the kidney and renal vein and the ureter leaves it. The cavity in the medullary portion of the kidney in which the renal calyces open and from where the renal pelvis starts is called as renal sinus.
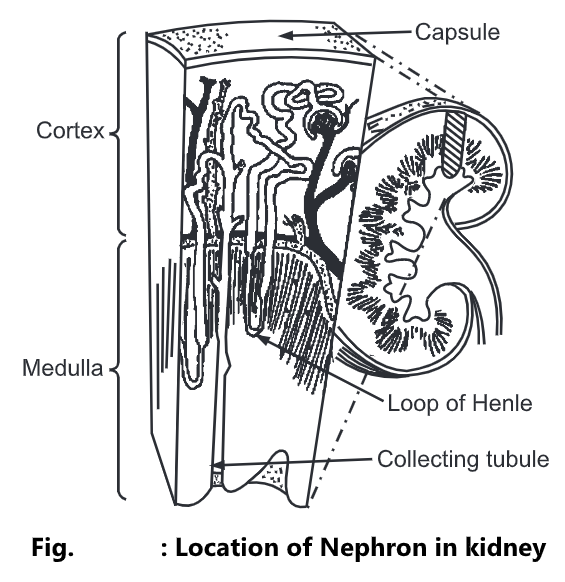
- The substance of the kidney in the outer reddish area is called the cortical substance (cortex) and in the inner reddish-brown area is called a medullary substance (medulla).
- Inside the renal capsule is the cortex and extensions of the cortex into the medulla, between the renal pyramids is known as the renal column.
- In the medulla, there are about 10-18 pyramid-shaped structures called renal pyramids. The pyramids are oriented so that their bases are facing towards the cortex and their tips project towards the hilum into the minor calyces of the renal pelvis.
- The tips (Papillae) of the pyramids project into a funnel-shaped minor calyx. Several minor calyces join together to form a major calyx.
- The major calyces join together to form the renal pelvis, which is an expanded upper end of the ureter.
Nephron
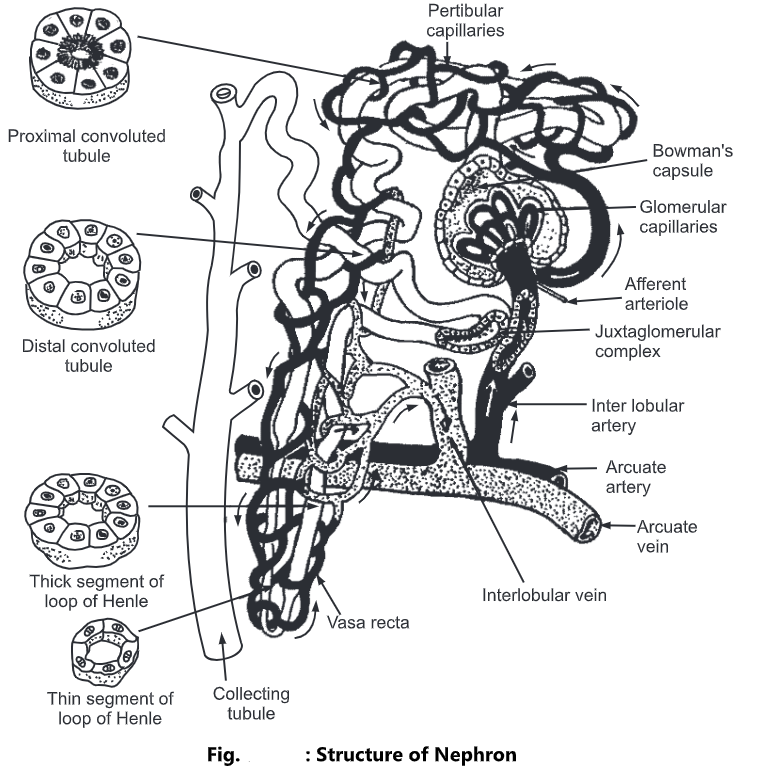
- The microscopic functional unit constituting the parenchyma (functional portion) of kidneys is known as Nephron. In each kidney, there are about one million nephrons. Each nephron consists of two parts, i.e. a renal corpuscle and a tubule.
- The proximal end of the closed tubule is indented to form a double-walled cup-shaped structure known as a glomerular capsule (Bowman’s capsule). There is a fine network of blood capillaries in close contact within the cup-shaped glomerular capsule, called glomerular capillaries.
- The glomerular capsule with glomerular capillaries is known as the renal corpuscle (Malpighian body).
- Beyond the glomerular capsule, the nephron forms a long tube, with convolutions and a loop, this part of the nephron is known as the tubule.
Renal Corpuscle
- These are located in the cortical region of the kidney. Some of the renal corpuscles located deep in the cortex, near the medulla of the kidney are termed as juxtamedullary (besides the medulla) and with their tubules in the medullary region are known as Juxtamedullary nephrons.
- The others are therefore known as cortical nephrons. The indentation of the tube at the glomerular capsule separates the outer wall of the glomerular capsule from the inner wall (visceral layer) by a capsular space.
- The inner layer of the capsule contains specialized cells called podocytes and adheres to the squamous cells of the endothelium of the blood capillaries that form the glomerular. The afferent arteriole, a branch of the renal artery enters the glomerular capsule.
- It divides and redivides to form a network of blood capillaries, these capillaries reunite to form efferent arteriole that leaves the glomerular capsule. This network of blood capillaries is known as glomerular capillaries.
- Under the electron microscope, spaces are evident between the cells in both the inner layer of the capsule wall and the endothelium of the glomerular. Through these openings, the substances get filtered from the blood and enter into capsular space. From capsular space, the filtered fluid passes into the renal tubule.
Renal Tubule
- It has three main parts: proximal convoluted tubule, loop of Henle, and distal convoluted tubule. The continuation of the glomerular capsule in the form of tube which is coiled is referred as proximal (close to capsule) convoluted tubule.
- The wall of tubule in this part is made up of a layer of thick cuboidal cells showing microvillus projecting into the lumen (brush border) of the tubule. This structural peculiarity of the cells is adapted for reabsorption of water as most water reabsorption occurs in this region.
- The proximal convoluted tubule continues further to form a ‘U’ shaped loop, called as loop of Henle and is situated in the pyramid of the medulla of kidney. The descending limb of this loop is formed of a thin squamous epithelium and is referred as thin segment of the loop.
- The ascending limb of the loop passes back into the cortex of the kidney. The wall of ascending limb is formed of cuboidal cells and is referred as thick segment of loop.
- The ascending limb of the loop on entering into cortex region comes into contact with the blood vessel called afferent arteriole (Branch of renal artery carrying blood to glomerular).
- At the point of contact, the cells of both tubule and blood vessel get modified and form a specialized structure called as ‘Juxtaglomerular apparatus.’
- The cells of this apparatus secrete rennin in response to decrease in blood pressure, which further leads to sequence of events causing rise in the blood pressure.
- Beyond the Juxtaglomerular apparatus the tubule further becomes coiled and is referred as distal convoluted tubule. The wall of the distal convoluted tubule is formed of single layer of cuboidal cells.
- The distal convoluted tubules of different nephrons join to form a common collecting tubule. About 10-25 collecting tubules open on the papilla of each pyramid and empty into a minor calyx. The cells forming wall of collecting tubule vary in shape and may be cuboidal or columnar in shape.
Blood Flow Through the Kidney
- The renal artery, a branch of the abdominal aorta carries a large amount of blood to each kidney. About 20 percent of the cardiac output is carried to the kidneys.
- This large blood supply to the kidneys is related to the excretion of waste and maintenance of homeostasis.
- After entering the kidney at the hilum the renal artery divides into several branches. These branches travel between the pyramids, i.e. through the renal columns as the interlobar arteries.
- At the boundary between medulla and cortex, the interlobar arteries form arching branches that run parallel to the surface of the kidney. These are the arcuate arteries. At intervals the arcuate arteries branch to form small interlobular arteries.
- The interlobular arteries divide into several afferent arterioles. Each afferent arteriole enters the cup shaped renal corpuscle where it divides to form network of capillaries called as glomerular. These capillaries reunite to form efferent arteriole which leaves the renal corpuscle.
- The efferent arteriole divides and redivides to form a network of capillaries that surrounds the proximal and distal convoluted tubules of the nephron. These capillaries are known as the peritubular capillaries.
- These capillaries reunite to form interlobular veins which in turn reunite to form successively the arcuate veins, the interlobar veins and renal vein that leave the kidney at hilum. Thus, the special feature of renal blood flow showing double capillary beds; first the glomerular and second the peritubular capillaries is related with the different stages involved in the formation of urine.
Physiology of Kidneys
Kidneys from urine by filtration and secretion of waste materials from the blood. In addition, the selective reabsorption by tubular cells contributes to the maintenance of homeostasis (regulatory activities of kidneys).
1. Formation of Urine
The nephrons of the kidney perform this function. Primarily, three processes are involved in the formation of urine, the glomerular filtration, tubular reabsorption and tubular secretion.
(a) Glomerular filtration:
- This occurs in the glomerular capsule. The barrier between internal portion of Bowman’s capsule and the blood present in the glomerular (the blood capillaries) act as an ultra filter.
- This barrier is composed of endothelial cells of capillaries, its basement membrane and the podocytes that form the inner portion of Bowman’s capsule.
- The ultra filter is highly permeable and allows free passage of water and solutes in blood plasma into the capsular space; forming the glomerular filtrate.
- The pore size of ultra filter is the only limitation for passage of solutes in blood plasma into the filtrate. Thus, the blood cells and plasma proteins are not filtered; hence except these constituents the composition of filtrate is same as that of plasma.
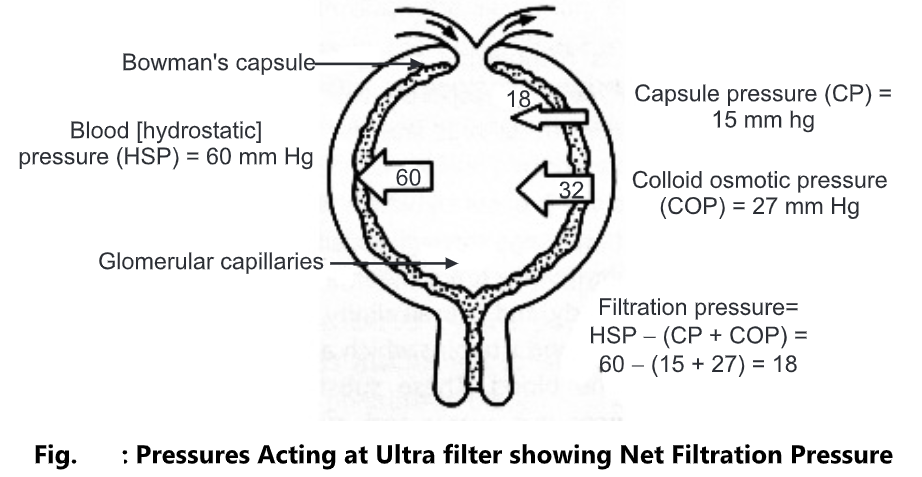
- Three different pressures are acting at this ultra filter. These are of different magnitude and the sum total of these is the net filtration pressure.
- The major with highest magnitude of these is the capillary blood pressure (hydrostatic pressure).
- It is about 60 mm Hg. The diameter of efferent arteriole is smaller than that of the afferent arteriole and this generates the hydrostatic pressure under the influence of which the filtration occurs.
- Two other pressures oppose this hydrostatic pressure; the oncotic pressure of blood plasma in capillaries; and the glomerular filtrate pressure.
- The plasma proteins are not filtered and they exert an oncotic (osmotic) force that opposes the filtration. This force is about 27 mm Hg. The glomerular filtration formed exerts pressure on the ultrafilter in opposite direction and is about 15 mm Hg. The resultant net filtration pressure is thus, 60 – (27 + 15)= 18mm Hg.
- The amount of filtrate produced is about 120 ml/min. Thus, about 170-180 liters of filtrate is formed within 24 hours in the case of normal adults.
- The urine output is 01 ml/min, i.e. about 01.5 liters in 24 hours; indicates that out of about 180 liters of filtrate; about 179 liters are reabsorbed by renal tubules.
Glomerular Filtration Rate (GFR)
- The amount of filtrate formed in both kidneys per minute is called GFR. It is 120 ml/min or 180 liters per day. GFR depends on Net Filtration Pressure (NFP) which in turn depends on capillary blood pressure (Hydrostatic pressure).
- The capillary hydrostatic pressure mainly depends on the difference in the diameter of afferent and efferent arterioles, and the systemic blood pressure. Although systemic blood pressure may vary, the pressure in the glomerular is maintained by alterations in the lumen (diameter) of the efferent arteriole as compared with the afferent arteriole.
- Thus, even in hypotension, the filtration continues so also in hypertension filtration occurs at a normal rate. This ability of kidneys to maintain constant blood pressure and GFR irrespective of changes in systemic blood pressure is referred to as renal ‘autoregulation.’
- The juxtaglomerular apparatus is responsible for renal autoregulation. The enzyme ‘rennin’ is secreted by juxtaglomerular cells in response to different stimuli; the unknown vasoconstrictor substance released from these cells and the hormone angiotensin II are all responsible for renal autoregulation function.
(b) Tubular reabsorption:
- It is the process by which the composition and volume of glomerular filtrate is altered during its passage through the tubule.
- The purpose of this process is to re-absorb the constituents of filtrate which are essential to the body, to maintain the fluid and electrolyte balance of the body and the alkalinity of the blood.
- The substances such as glucose, amino acids, fatty acids, and vitamins which are more useful to the body are completely re-absorbed back into the blood.
- These substances are described as high threshold substances. Some substances, e.g. water and mineral salts are reabsorbed in varying amounts according to the physiological need of the body.
- Waste products such as urea and uric acid are absorbed only to a slight extent. These are called low threshold substances. Some substances, e.g. creatinine sulfate are not at all reabsorbed.
- The tubular cells are responsible for reabsorbing materials from filtrate back into the blood. Reabsorption occurs by both active and passive diffusion and even by osmosis.
- The active process involves carriers within tubular cells; and transports only a limited amount of material per unit time.
- If the substance to be transported is present in excess of the limits of transportation such excess substance will appear in the urine.
Tubular reabsorption varies in different parts of the tubule as shown in the table below.
| Tubular reabsorption | ||
| Part of tubule | Mechanism of reabsorption | Substance reabsorbed |
| 1. Proximal convoluted tubule. | a. Active transport | Glucose, amino acids, vitamins, bicarbonates, sodium. |
| b. Passive diffusion | Chloride, sulphate, phosphate and urea. | |
| c. Osmosis | Water (obligatory water reabsorption). | |
| 2. Loop of Henle | a. Active transport | Chlorides (Cl–) and Potassium (K+). |
| b. Passive diffusion | Sodium (Na+) – first -by Passive diffusion into the tubular cell and then by active transport to blood. | |
| 3. Distal convoluted tubule and collecting tubule. | a. Active transport
|
Sodium (Na+ ) in exchange for K+ or H+ . |
| b. Hormonal influence | Facultative reabsorption of water. | |
(c) Active secretion: Tubular cells actively secrete certain substances into the filtrate. This secretion is aimed at getting rid of certain materials and controlling blood pH. The substances secreted by tubular cells include Potassium (K+), Hydrogen (H+) ammonium ions (NH4+) and creatinine.
2. Water Balance
Water constitutes about 60 percent of adult human body weight. It is distributed in the body in three main compartments, i.e.
| Blood plasma
Interstitial fluid Intracellular fluid |
5%
11% 44% |
The figures are in terms of adult male |
- Water is taken into the body through the alimentary canal and a small quantity is also produced by the metabolic process in the body.
- Water is excreted from the body in the expired air, as a constituent of feces, as sweat, through the skin, and through urine.
- The amount of water excreted in expired air and in feces is fairly constant. Water excreted in the sweat is associated with the maintenance of body temperature.
- The balance between intake and output is maintained by the kidneys. Normally, the fluid output is directly related to fluid intake.
- Water loss through the kidneys is rigorously controlled and varies from 1000-1500 ml in 24 hours. This output is mainly controlled by the antidiuretic hormone (ADH).
- This hormone is produced and released into the blood by the posterior lobe of the pituitary gland. The osmotic pressure of blood is always maintained constant. Any increase or decrease in the intake of water, affects the osmotic pressure of blood.
- If the osmotic pressure of the blood is raised, the osmoreceptors in the hypothalamus are stimulated. There is a close link between the hypothalamus and the posterior lobe of the pituitary gland.
- The stimulation of osmoreceptors in the hypothalamus results in increased output of ADH by the pituitary gland. Conversely, if the osmotic pressure of blood is reduced, the release of ADH in the blood is reduced.
- The ADH acts on the tubules of the kidneys which increases the permeability of distal and collecting tubules. This results in an increase in the reabsorption of water from the tubule into the circulating blood.
- An increase in the concentration of dissolved substances in the blood increases the production of ADH, resulting in the reabsorption of water which dilutes the blood. The effect of diluting the blood is to reduce the amount of ADH produced. The cyclic effect maintains the concentration of ADH in the blood within narrow limits.
- Although the antidiuretic hormone is an important means by which the water balance of the body is maintained, it is not the only one. If there is an excess amount of any dissolved substance in the blood, it is excreted through the kidneys and excess of water is excreted with it; for example, in case of untreated diabetes mellitus. Also, if excess amount of electrolytes have to be excreted from the body, the amount of water required for this purpose is increased. This may lead to dehydration, inspite of increased production of ADH, but it is usually accompanied by acute thirst and increased water intake.
3. Electrolyte Balance
Changes in the concentration of electrolytes in the body may be due to changes in the amount of water or the amount of electrolytes. Sodium is the most common of the cations that exists in the extracellular fluid. As it is excreted through urine, its balance in the body is maintained by kidneys. When the amount of sodium is decreased, aldosterone production is increased and an increased amount of sodium is reabsorbed by kidneys. The secretion of aldosterone is influenced by ACTH from the pituitary gland by a fall in the concentration of sodium in the blood and the rennin produced in the kidneys.
4. Maintenance of the Blood Pressure
The Juxtaglomerular cells in the kidney are responsible for this function. When the blood pressure decreases, it causes the release of hormone rennin by the kidneys. Renin reacts with globulin in the blood and forms angiotensinogen which in turn forms angiotensin-l. It stimulates the adrenal cortex to produce the hormone aldosterone which causes increased reabsorption of sodium. This is followed by reabsorption of water; the blood volume increases, thereby increasing the blood pressure. The angiotensin-I is converted into angiotensin-II by the enzymes in the lungs. Angiotensin-II is a powerful vasoconstrictor and increases blood pressure. Thus, the blood pressure is maintained.
|
Components and Characteristics of Normal urine |
||
| Components | Percent Composition | Amount in 24 hours urine sample |
| 1. Water | 95 | 950-1430 ml |
| 2. Urea | 02 | 20-35 g |
| 3. Creatinine | 0.075 | 01-01.5 g |
| 4. Uric acid | 0.05 | 0.5-0.8 g |
| 5. Sodium ions | 0.35 | 03.5-06 g |
| 6. Potassium ions | 0.15 | 02-03.5 g |
| 7. Calcium ions | 0.015 | 0.01-0.3 g |
| 8. Ammonium ions | 0.04 | 0.08-0.5 g |
| 9. Magnesium ions | 0.006 | 0.06-0.08 g |
| 10. Chloride ions | 0.6 | 06-09 g |
| 11. Phosphate ions | 0.15 | 01.5-02.5 g |
| 12. Sulphate ions | 0.18 | 01-015 g |
| 13. pH | – | 04.8-07.4 |
| 14. Specific gravity | – | 01.016-01.02 |
| 15. Volume | – | 1000-1500 ml |
Ureter
- The ureter commences from hilum of the kidney as upper funnel shaped end known as renal pelvis.
- The collecting ducts of nephrons open into papillary ducts which in turn open into minor calyces.
- The minor calyces join to form major calyx; two or three such major calyces unite to form the renal pelvis.
- The renal pelvis extends downwards as a small tube of 04-05 mm in diameter. Each ureter is about 25-30 cm in length and opens into urinary bladder.
- The ureter pass obliquely through the wall of urinary bladder. When bladder is full of urine the pressure compresses the urethral openings and prevents the backflow of urine into ureter.
- Three coats of tissues that form the ureter are the outer fibrous coat, middle muscular coat and an inner mucous lining.
- The mucous lining is composed of transitional epithelium and mucous secreted by its cells act as protective coat over those cells, preventing their contact with urine. The peristaltic contractions of muscle coat propel the urine to the urinary bladder.
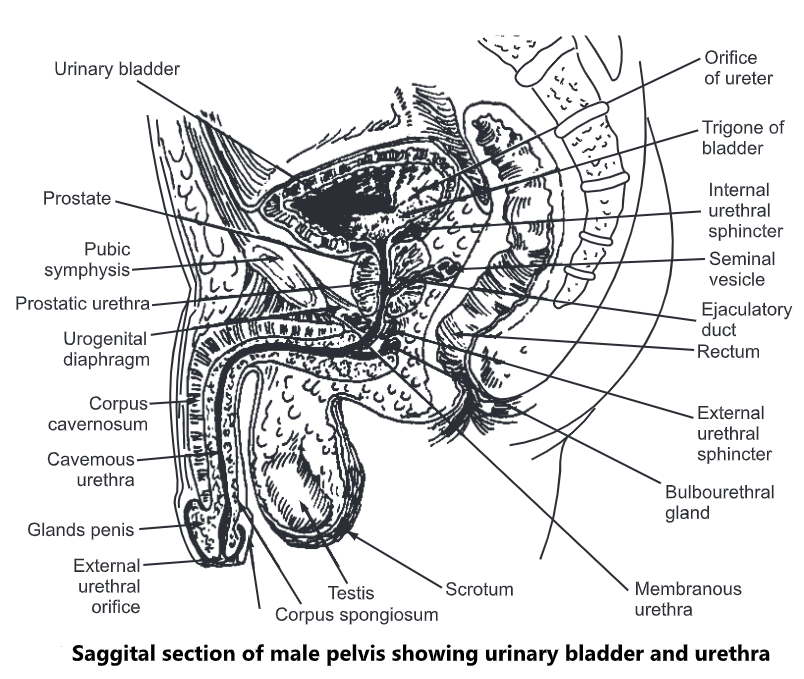
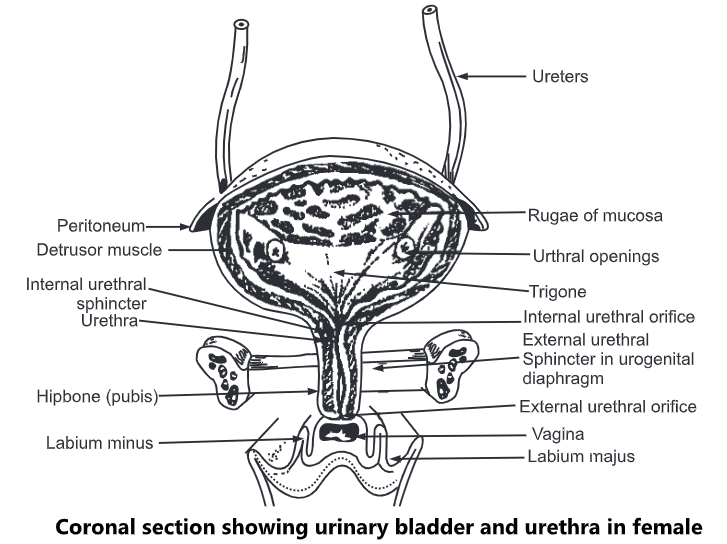
Urinary Bladder
- It is a hollow muscular organ situated in the pelvic cavity posterior to the symphylids pubis, anterior to rectum in male and anterior to neck of uterus and vagina in female.
- Its shape depends on amount of urine it contains; when empty it collapses and when accumulation of urine occurs it goes on distending. When it is full of urine, it is ovoid in shape and rises considerably up in the abdominal cavity.
The urinary bladder has four coats:
(1) The innermost is the mucous lining formed of transitional epithelium, which shows folds (rugae) except in small triangular part formed between the openings of ureter and the orifice of urethra. This triangular part is known as trigone. The folds allow the distension of bladder as urine accumulates in it.
(2) The submucous coat is made up of connective tissue that connects inner mucous coat with the outer muscular coat.
(3) The muscle coat has three layers of smooth muscles: inner longitudinal, middle circular and outer longitudinal. At the urethral orifice the circular muscle forms an internal urethral sphincter.
(4) The outermost serous coat is a reflection of peritoneum and covers only superior surface and the upper parts of lateral surfaces of bladder.
The bladder is supplied by autonomic nerves from both the branches of autonomic nervous system (craniofacial and thoracolumbar). The reflex centres of these fibres are located in the midbrain, anterior pons and hypothalamus. The impulses froms these nerves are responsible for contraction of bladder and relaxation of internal urethral sphincter.
The bladder functions as a reservoir for urine.
Urethra
- The urethra is a muscular tube that extends from inferior surface of urinary bladder and carries urine to the exterior of the body. At the pelvic floor when it passes through the muscle, (urogenital diaphragm) it is surrounded by the external urethral sphincter.
- In females, it is a narrow membranous canal extending from bladder to external orifice the meatus, and about 03.8 cm in length.
- It is placed obliquely downwards and forwards along the anterior wall of vagina. The meatus is the narrowest part and is located between the clitoris and the opening of the vagina.
- The walls of the urethra have three coats:
(1) Outer muscular coat which is continuous with that of the bladder.
(2) Middle thin layer of spongy tissue and
(3) Inner mucous coat.
- The male urethra is about 20 cm long and depending on the location it is described as having three parts:
(1) Prostatic; which runs vertically through prostate gland,
(2) Membranous which extends between prostate to urogenital diaphragm.
(3) The cavernous portion, which extends from membranous to the urethral meatus.
Micturition
- The act of passing the urine to the exterior is called as micturition. It is carried out by both voluntary and involuntary nerve impulses.
- When urine accumulates in the bladder, sufficiently (about 300 ml) it results into stretching of bladder wall and stimulates the nerves to initiate sensory impulses transmitted to the lower portion of the spinal cord.
- These impulses by way of sensory tracts to the cortex initiate a conscious desire to expel urine. By way of micturition reflex, of which the center is in the sacral spinal cord; the bladder muscles are stimulated to contract and the internal urethral sphincter to relax. By way of sensory tracts to the cortex, the conscious desire to expel urine is felt.
- These higher centers in the brain can voluntarily control the contraction or relaxation of the external urethral sphincter. When the voluntarily external urethral sphincter is relaxed, the micturition occurs.
Pathophysiology of Renal Diseases
- Glomerulonephritis is an inflammatory condition, possibly of allergic origin. Glomeruli are the main targets. Oedema may be present in both the acute and sub-acute stages of nephritis.
- This stage is called dry nephritis. The cause of oedema is as follows : Two, more or less equal but opposite, forces are always at work in the fine capillaries.
(a) Blood pressure, which tries to force the fluid part of the blood through the vessel wall into the tissues.
(b) The osmotic pressure of the blood proteins which holds the fluid back with the vessels.
- In nephritis, the blood proteins are seriously diminished because of albuminuria. This reduces the osmotic pressure. As a result, more fluid is forced through the vessel wall into the tissues resulting in oedema.
- If the site of damage is tubules, rather than glomeruli, it is called tubular nephrosis. It involves the combination of albuminuria and massive oedema.
- Pyelonephritis involves inflammation of the kidney and the renal pelvis. The inflammation is primarily of the interstitial tissue.
- The case is an infection by pyogenic bacteria, particularly E. coli, Streptococci and Staphylococci. It is one of the commonest forms of renal diseases. In chronic conditions, hypertension may develop.
- Hypertension caused by glomerulonephritis or pyelonephritis is called secondary hypertension.
- Urinary calculus is a stone that is formed in the urinary tract. It may be formed either in the kidney or in the bladder. The symptoms include pain, the passage of pus and blood through urine, and evidence of renal failure.
Oedema
- All the cells in the body are bathed in the tissue fluid. It serves as a medium of exchange between blood plasma and the cells.
- The tissue fluid is derived from the plasma of the blood. As the walls of blood capillaries are thin, some of the fluid passes out into the space between the tissue cells. This occurs by means of diffusion and by capillary hydrostatic pressure.
- Another force, called protein osmotic pressure is formed by the plasma protein which acts as a pulling force to hold the fluid in the vessel as well as to attract fluid in. This opposite force prevents undue loss of fluid from the capillaries.
- As blood moves through the capillary network and some fluid is lost in the tissue space, the plasma protein concentration is slightly increased and hence the pulling force is increased.
- As a result, the water and crystalloids re-enter the capillaries colloids with water and enter the lymph capillaries. Thus, normally there is a delicate balance between the fluid leaving and re-entering the capillaries.
- The disturbance in this balance causes a decrease in fluid return in the capillaries results in the excess accumulation of tissue fluid called oedema. The oedema may arise from the following reasons —
(1) Excessive mechanical hydrostatic pressure in the capillaries, if venous drainage is blocked;
(2) Decrease in osmotic pressure due to insufficient plasma proteins;
(3) Blockage of lymphatics;
(4) Damage to the capillary walls so that plasma proteins leak out into tissue spaces and
(5) An important factor causing oedema is the inability of kidneys to excrete sodium.
The basic treatment for oedema is the administration of diuretics, which are drugs that increase the quantity of urine production.